J Oral Pathol Med:沙利度胺在复发性口角炎维持治疗中的更优剂量
2022-02-11 MedSci原创 MedSci原创
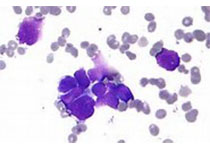
复发性咽喉炎(RAS)是最常见的口腔黏膜疾病,无溃疡期是患者的主要关注点。沙利度胺已被证明是治疗RAS的有效系统性药物,但有必要进行试验以评估各种维持剂量的疗效。
复发性咽喉炎(RAS)是最常见的口腔黏膜疾病,无溃疡期是患者的主要关注点。沙利度胺已被证明是治疗RAS的有效系统性药物,但有必要进行试验以评估各种维持剂量的疗效。为此,近日发表于J Oral Pathol Med的一项随机对照的临床试验探究了不同维持剂量的沙利度胺治疗RAS的疗效和安全性。

该项随机试验采用了两阶段的设计。首先,所有125例RAS患者接受泼尼松,起始剂量为15mg/d,为期一周,作为初始治疗药物。其次,实验组的100例RAS患者接受沙利度胺(50 mg/d vs. 25 mg/d)作为维持用药,观察其疗效和安全性。
结果显示,在第四和第八个周末的维持用药期间,两种剂量(50和25mg/d)的沙利度胺在减少溃疡发生率、溃疡数量和溃疡疼痛方面均是相当的(均P>0.05)。值得注意的是,使用25mg/d沙利度胺组患者使用8周的无溃疡期比其他组别更长(平均,>3个月)(所有P<0.05)。重要的是,25mg/d沙利度胺组患者的总不良事件明显少于使用50mg/d组的患者(P < 0.001)。此外,50 mg/d沙利度胺组患者对各种唾液细胞因子水平的影响并不优于25 mg/d沙利度胺组(p>0.05)。
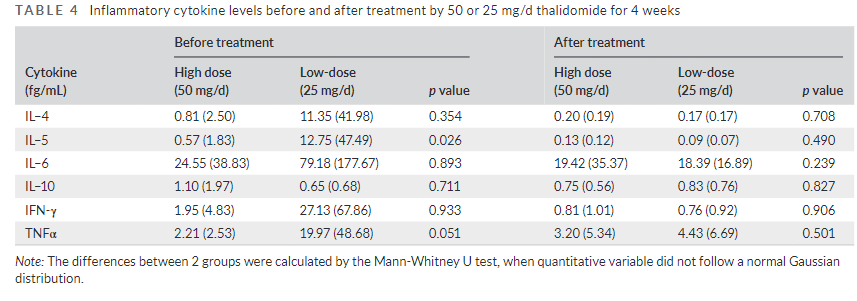
综上所述,这项剂量优化研究调查了大剂量(50mg/d)和小剂量(25mg/d)沙利度胺在RAS维持治疗中的有效性和安全性,结果发现25mg/d的沙利度胺给药8周,对延长RAS的RI(平均,>3个月)有长期效果,且安全性更好。
原始出处:
Yiwen Deng, et al., A Randomized controlled clinical trial on dose optimization of thalidomide in maintenance treatment for recurrent aphthous stomatitis. J Oral Pathol Med. 2022 Jan;51(1):106-112. doi: 10.1111/jop.13259.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Pathol#
46
#复发性#
43
#Oral#
39
#Med#
33