JNNP:丘脑神经刺激改善特发性全身性癫痫发作控制
2022-03-10 MedSci原创 MedSci原创
这个数字的五分之一大约是在美国,有100万癫痫患者被诊断为特发性全身性癫痫(IGE)。其中约10%–40%的患者从未通过药物获得足够的癫痫控制,
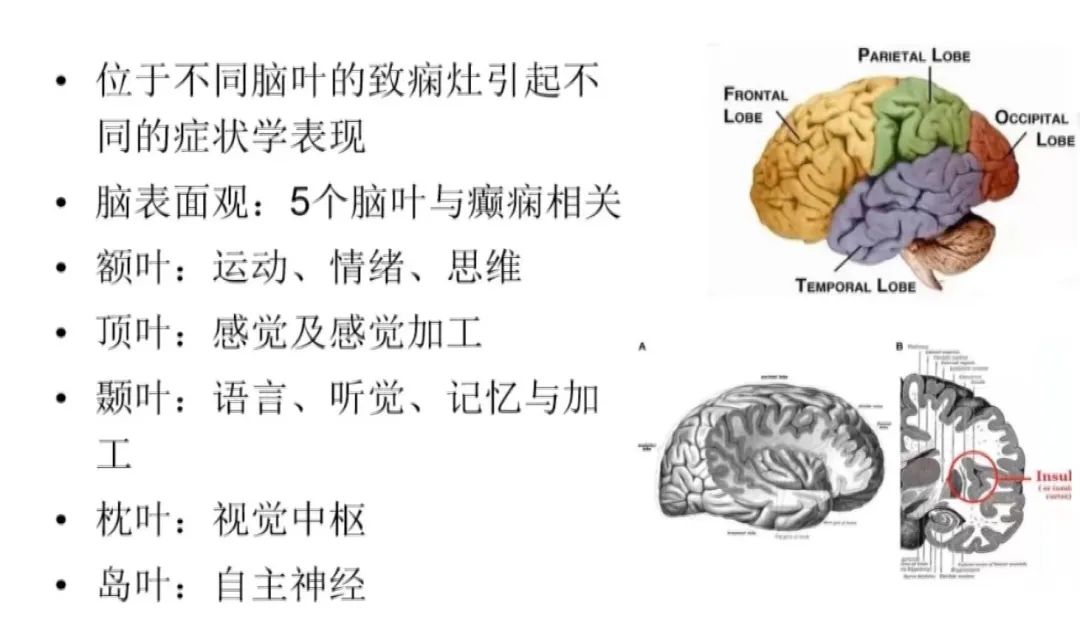
这个数字的五分之一大约是在美国,有100万癫痫患者被诊断为特发性全身性癫痫(IGE)。其中约10%–40%的患者从未通过药物获得足够的癫痫控制,全身强直阵挛(GTC)发作和肌阵挛发作类型增加了耐药性的风险,对生活质量和健康造成重大不利影响。与局灶性癫痫不同,IGE患者不适合手术切除和潜在治愈。脑刺激是一种外科治疗方法,有望减轻药物难治性IGE患者的癫痫发作负担。
与传统的DBS相比,闭环脑刺激使用可编程的检测和刺激来根据患者的个体神经生理学定制治疗,并已证明局灶性癫痫发作的频率和严重程度的降低优于DBS或迷走神经刺激(VNS)。 NeuroPace RNS系统(RNS)是唯一的闭环设备美国食品和药物管理局(FDA)批准用于局灶性癫痫患者。之前的病例报告显示,一名在CM区接受RNS治疗的IGE患者在18个月时癫痫发作频率和严重程度显著降低。在这里,介绍了在一个中心接受CM-RNS治疗的四名IGE患者的最初系列的2年结果。本文发表在《神经病学,神经外科学和精神病学杂志》上().
受试者患有抗药性癫痫(普遍诊断为IGE),并根据多学科癫痫外科会议的建议进行了丘脑RNS植入。受试者通过机构审查委员会(IRB)批准的癫痫手术数据库进行回顾性研究,他们同意纳入该数据库。根据多学科癫痫团队的专家意见,植入RNS治疗泛发性癫痫不需要IRB审查,目的是为这些耐药患者提供减少癫痫发作的最佳潜在治疗选择。在全身麻醉下,接触深度导线的接触长度为2.0 毫米,接触间隔为3.5毫米 使用机器人立体定向辅助(ROSA,Zimmer Biomet)植入。将患者仰卧放置于经额入路点,使用牢固连接在机器人底盘上的Leksel立体定向框架进行头部固定,并通过在术前基于CT的Leksell框架三维模型上选择点进行共同登记。植入后,RNS被设置为在无刺激的情况下记录颅内EEG(iEEG)。
患者植入位置与脑电记录
患者经历了发作持续时间和严重程度降低(Engel 1B、IC、IIA和IIIA级),生活质量显著改善。经过至少2年的治疗,结果是持久的。在连续的编程阶段,所有患者的检测准确率总体上从平均96.5%下降到88.3%。大多数用于传递刺激的电极位于CM(7/10),其次是后背腹外侧(2/2)、后腹后外侧(3/4)和后腹外侧(2/3)。在所有患者中,刺激在0.2到2.0 mA之间变化,振幅仅在连续时间内增加。颅内脑电图记录的原始百分比为24.8%、1.2%、7.6%和8.8%。

癫痫发作趋势
植入了第一批接受闭环丘脑刺激的IGE患者,并评估了超过2年的癫痫发作结果 多年的治疗。CM-RNS通过降低癫痫发作频率和严重程度,在该队列中的所有患者中产生了强大而持久的治疗反应,从而使生活质量得到明显改善。四名之前患有顽固性癫痫的患者中,有两名获得了驾驶执照,能够维持全职工作和长期关系。这些结果在两年多的时间里具有重大的前景 。
对CM区进行闭环刺激可能会显著改善抗药性IGE患者的癫痫发作控制和生活质量。最佳检测和刺激位置及参数仍然是一个热点研究领域。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#脑神经#
40
#特发性#
37
#神经刺激#
43
#丘脑#
36
#丘脑#
53