Sci Adv: 匹兹堡大学:新的小蛋白药物可减轻中风的后遗症,保护大脑
2020-07-05 Lauren 转化医学网
脑卒中(Stroke)俗称中风,包括缺血性脑卒中(脑梗死)和出血性脑卒中(脑实质出血、脑室出血、蛛网膜下腔出血)。具有发病率、致残率、复发率和死亡率高的特点。脑卒中是中国居民排名第一位的死亡原因。缺血
脑卒中(Stroke)俗称中风,包括缺血性脑卒中(脑梗死)和出血性脑卒中(脑实质出血、脑室出血、蛛网膜下腔出血)。具有发病率、致残率、复发率和死亡率高的特点。脑卒中是中国居民排名第一位的死亡原因。缺血性卒中占所有卒中的75%-90%,出血性卒中只占10-25%。且中风患者的后遗症很难治疗。
匹兹堡大学大脑研究所的神经科学家发现了一种新型药物,可以在中风期间和中风后保护大脑。
在7月1日发表在《科学进展》(Science Advance)杂志上的一项研究表明,受损的神经元如果不遵循导致细胞死亡的生化途径,仍然可以存活。
皮特医学院科学家培训项目的医学生、该研究的第一作者安东尼·舒连(Anthony Schulien)表示,“在临床实践中,没有任何药物能够阻止中风后发生的细胞死亡。这些实验为药物靶向提供了令人振奋的早期证据,我们希望有一天能将这些证据应用到患者身上。”
皮特医学院神经生物学教授、资深作者伊莱亚斯·艾泽曼(Elias Aizenman)博士解释说,中风的发生是因为脑血栓阻塞了血管,阻碍了血液和氧气到达神经元并杀死它们。附近被称为中风半暗区的神经元也可能功能障碍,在数小时或数天后死亡,即使它们的血氧供应只是轻微或短暂地减少。
艾泽曼表示:“我们也在寻找防止其他神经元死亡的方法,如果我们能做到这一点,康复可能会得到改善,我们可能就能更好地帮助那些血栓在无法进入血管或不能及时到医院进行早期干预的中风患者。有了正确的药物,我们也可能能够在病人到达医院之前减缓已知的中风的进展。”

在之前发表的研究中,艾泽曼的研究小组显示,细胞膜上钾离子通道Kv2.1和合成素蛋白质之间的相互作用促使钾离子从神经元中泄漏出来,引发细胞死亡。他们发现使用一种叫做TAT-C1aB的实验化合物可以通过干扰合成素和Kv2.1的相互作用来防止细胞死亡。
在这项新的研究中,研究人员确定了神经元细胞膜中两种类型的Kv2.1通道。一个通道通常与细胞兴奋性有关,而另一个通道允许额外的、新的Kv2.1通道进入细胞膜,促进钾的释放并最终导致神经元细胞死亡。
有了这些知识,科学家们创造了一种名为TAT-DP-2的新小蛋白质,它可以破坏这些新通道进入细胞膜的通道,使钾离子留在细胞内,阻止细胞死亡的生化途径。
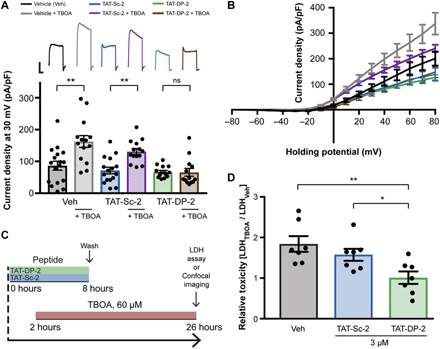
TAT-DP-2在体外抑制促凋亡Kv2.1电流冲击并具有神经保护作用

小鼠腹腔注射TAT-DP-2可减少脑梗死体积
中风后注射TAT-DP-2的小鼠中风损伤区域较小,长期神经功能优于未注射的小鼠。使用Kv2.1的两种完全不同的方法可以改善中风的结果,这表明了针对该通道的神经保护药物的前景广阔。
原始出处:Anthony J. Schulien, Chung-Yang Yeh, Bailey N. Orange, et al. Targeted disruption of Kv2.1-VAPA association provides neuroprotection against ischemic stroke in mice by declustering Kv2.1 channels. Science Advances 01 Jul 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#匹兹堡大学#
35
荧光图好专业
87
#后遗症#
39
中风是俗称,应该称为缺血性卒中吧
38
😁
68