J Endod:急性根尖周脓肿合并自身免疫性肝炎患者的治疗效果:一例病例报告
2019-11-29 lishiting MedSci原创
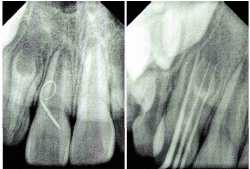
这篇研究的目的是报道一例临床病例:诊断为严重根尖周脓肿合并自身免疫性肝炎(AIH)(服用免疫抑制药物以及二磷酸盐)。 患者为32岁的非洲黑人后裔,因咀嚼时右下第二前磨牙区域肿胀不适、有异物感且体积增大而急切寻求口腔手术治疗。经口内检查和X线影像观察,患者诊断为牙髓坏死合并急性根尖周脓肿。由于其罹患AIH并服用皮质类固醇和双磷酸盐药物(阿仑膦酸),考虑到患者的全身状态,对他实施最小的侵入性
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗效果#
27
#根尖周脓肿#
33
#肝炎患者#
27
#病例报告#
33
#脓肿#
30
好好好好好好
83
好
71
谢谢梅斯提供这么好的信息,学到很多
47
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
53
学习了谢谢分享
72