J Rheumatol:TNF抑制剂在反应性关节炎中的疗效和安全性
2020-03-01 xiangting MedSci原创
使用TNFi治疗ReA是安全有效的,但治疗时间经常延长。亟需ReA的进一步临床试验。
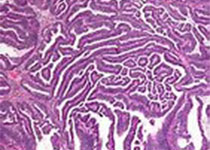
反应性关节炎(ReA)是一种由细菌感染引发的脊椎关节炎。在非甾体类抗炎药和常规合成疾病改善抗风湿药治疗失败的病例中,已开始使用诸如肿瘤坏死因子抑制剂(TNFi)的生物制剂。但是,关于这些药物在ReA中疗效和安全性的证据有限。这里报道了接受TNFi治疗冰岛ReA患者的特征、结局和安全性。
研究人员使用冰岛国家生物治疗数据库(ICEBIO)进行了一项观察性队列研究,并对电子病历数据进行回顾性研究作为补充。使用疾病活动性评分和ICEBIO内的标准化问卷对药物疗效进行评估;使用ICEBIO和电子病历数据评估安全性。
数据库中登记了38例ReA患者。8例患者在症状发作1年内接受了TNFi治疗。在6个月和18个月时,C反应蛋白(CRP)、压痛和肿胀关节、疼痛和疲劳的视觉模拟量表、疾病活动性评分28关节计数CRP(DAS28CRP)、临床疾病活动性指数(CDAI)和健康评估问卷(HAQ)评分均显著降低。71%至90%的患者被视为治疗反应者。由于缓解,2例患者能够停止使用生物制剂。在生物制剂治疗的303患者年中(平均8年,范围1-15),发现有6例因感染入院。
使用TNFi治疗ReA是安全有效的,但治疗时间经常延长。亟需ReA的进一步临床试验。
原始出处:
Bjarni
Thorsteinsson. Outcomes and safety of TNF inhibitors in reactive arthritis: A
nationwide experience from Iceland. J Rheumatol. February 2020.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#反应性#
34
#抑制剂#
42
#疗效和安全性#
33
#关节炎#
42
#TNF#
60
谢谢梅斯提供这么好的信息,学到很多
58