NEJM:MRSA 携带者出院后如何管理?
2019-03-29 杨中华 脑血管病及重症文献导读
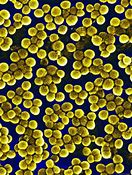
在美国每年超过8万例耐甲氧西林金黄色葡萄球菌(Methicillin-resistant Staphylococcus aureus,MRSA)侵袭性感染。它是皮肤、软组织和手术相关感染的最常见原因。出院后6个月内侵袭性 MRSA 感染率最高。
在美国每年超过8万例耐甲氧西林金黄色葡萄球菌(Methicillin-resistant Staphylococcus aureus,MRSA)侵袭性感染。它是皮肤、软组织和手术相关感染的最常见原因。出院后6个月内侵袭性 MRSA 感染率最高。
降低 MRSA 携带和预防感染的方法包括卫生学和环境净化的教育以及鼻腔莫匹罗星和氯已定洗浴去定植。研究显示去定植能够降低外科手术部位感染、皮肤感染复发和 ICU 感染。
2019年2月来自美国的Susan.S. Huang等在NEJM 上公布了Project CLEAR试验结果,目的在于探讨 MRSA 定植患者在出院后采用去定植联合卫生学教育降低 MRSA 感染是否优于单独卫生学教育。
该研究为多中心,随机对照试验,纳入的患者为 MRSA 定植者(携带者)。纳入的患者随机给予卫生学教育联合去定植或单独卫生学教育。去定植包括氯已定漱口、洗浴或淋浴以及鼻腔莫匹罗星外用5次,每个月两次,持续6个月。随访1年。主要终点为 MRSA 感染(按照 CDC 定义)。二级终点包括 MRSA 感染、任何原因感染和感染相关住院。
结果发现,在符合方案人群中,教育组和去定植组MRSA感染率分别为9.2%和6.3%;84.8%的 MRSA 感染进行了住院治疗。教育组和去定植组任何原因感染率分别为23.7%和19.6%;85.8%的感染进行了住院治疗。去定植组 MRSA 感染的风险(hazard)明显低于教育组(HR, 0.70; 95% CI, 0.52 to 0.96; P = 0.03; number needed to treat to prevent one infection, 30; 95% CI, 18 to 230);这个较低的风险带来的好处是更低的因 MRSA 感染住院风险(HR, 0.71; 95% CI, 0.51 to 0.99)。去定植组组发生任何原因感染(HR, 0.83; 95% CI, 0.70 to 0.99)和感染相关住院(HR, 0.76; 95% CI, 0.62 to 0.93)的可能性更低;不过应该慎重解读二级终点的治疗作用,因为未预先调整多重比较。In as-treated analyses,对于去定植组完全依从方案的参与者,MRSA 感染率(44%)(HR, 0.56; 95% CI, 0.36 to 0.86)和任何原因感染(40%)(HR, 0.60; 95% CI, 0.46 to 0.78)皆比教育组更低。总副作用率为4.2%(皆较轻)。
最终作者认为出院后采用氯已定和莫匹罗星MSRA 去定植能够降低30%的 MRSA 感染风险(vs 教育)。
原始出处:Susan S. Huang, Raveena Singh, James A. McKinnell, et al. Decolonization to Reduce Postdischarge Infection Risk among MRSA Carriers. N Engl J Med 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mRS#
49
#携带者#
34
#MRSA#
33
谢谢分享
75
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
62