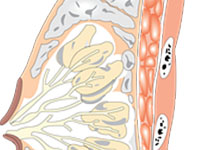
Nat Commun:转移性乳腺癌研究又有新进展
2017-04-25 佚名 来宝网
来自于Jules Bordet研究所-布鲁塞尔自由大学、比利时法兰德斯生物中心(VIB)和鲁汶大学的研究人员于4月21日发布了一项重要研究报告,该报告对乳腺癌的进展有了更深一步的分析,它将对转移性乳腺癌患者的治疗产生一定影响。报告的研究数据来源于对病人的尸体解剖,这种获得研究数据的方式还是首次。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#COMMUN#
35
#Nat#
0
可以可以
1
#转移性#
34
不错
55
在乳腺癌复发时,至少对一处转移病变进行活检并分析,尽可能的给出病灶的特定基因组谱。
46
学习了
52
进展不错 值得研究
48
继续学习。
24
太棒了,又进一步了,值得分享!
22