Pancreatology:术中胰液淀粉酶水平可作为胰十二指肠切除术后胰瘘的简单预测指标
2021-04-08 MedSci原创 MedSci原创
胰十二指肠切除术(PD)后,胰腺的残留的软组织通常被认为是术后胰瘘(POPF)发生的危险因素。但是,其评估是偏主观的。因此,本项研究的目的是评估术中胰液淀粉酶
胰十二指肠切除术(PD)后,胰腺的残留的软组织通常被认为是术后胰瘘(POPF)发生的危险因素。但是,其评估是偏主观的。因此,本项研究的目的是评估术中胰液淀粉酶水平作为PD后POPF的危险因素的意义。
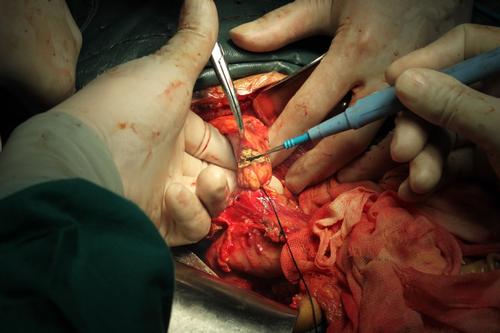
这项研究纳入了75名在2014年11月至2020年4月期间在当地医院接受PD治疗的患者。研究通过收集术后胰腺质地,术中胰液淀粉酶水平,病理学评估结果来评估这些变量与POPF发生率之间的关系。
结果显示有23名患者出现了POPF。POPF的重要预测指标是非导管腺癌(p <0.01),胰腺残留组织较多(p <0.01),术中失血量高(p <0.01),术中胰液淀粉酶水平高(p <0.01)和胰腺纤维化低(p <0.01)。多变量分析显示,POPF的重要独立预测因素是术中失血量高(p <0.01)和术中胰液淀粉酶水平高(p = 0.02)。接收者操作特征(ROC)分析显示,胰液术中淀粉酶水平的临界值为2.17×105 IU / L(曲线下的面积= 0.726,灵敏度= 95.7%,特异性= 50.0%)可以很好地区分胰瘘患者和非胰瘘患者。
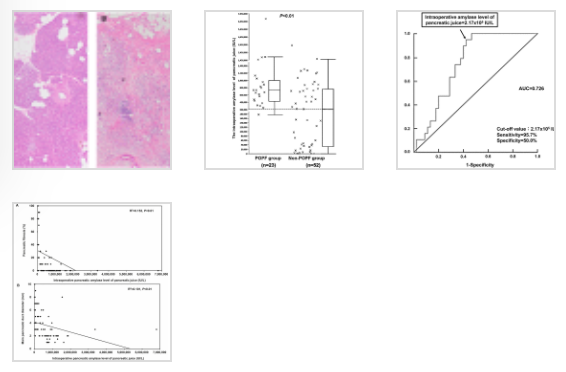
图:术中胰淀粉酶水平与术后胰瘘的关系
作者最后说道:术中胰液淀粉酶水平可以是PD术后发生POPF的可靠的预测指标。
原始出处:
Kenei Furukawa. Et al. Intraoperative amylase level of pancreatic juice as a simple predictor of pancreatic fistula after pancreaticoduodenectomy. Pancreatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#切除术#
41
#十二指肠#
55
#预测指标#
33
#淀粉酶#
43
#胰瘘#
45
#CRE#
46