Cochrane Database Syst Rev:抗抑郁药缺乏安全停用的证据
2021-04-25 MedSci原创 MedSci原创
Cochrane的一篇综述强调,迫切需要优质的证据来告知医生如何安全有效地停用抗抑郁药。
Cochrane的一篇综述强调,迫切需要优质的证据来告知医生如何安全有效地停用抗抑郁药。
一组国际研究人员评估了一些随机对照试验,这些试验比较了使用抗抑郁药治疗抑郁或焦虑至少6个月的患者停用和继续使用抗抑郁药的方法。但是由于现有研究中证据的不确定性,该团队对这些方法的疗效和安全性没有得出确切的结论。比利时根特大学临床药理学组的第一作者Ellen Van Leeuwen认为有超过1000项研究着眼于开始使用抗抑郁药物,但只有33项试验研究如何阻止它们。很明显,这个领域需要紧急关注。
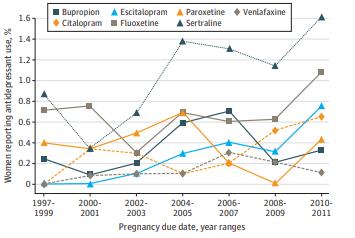
指南建议,在症状改善后,抗抑郁药应继续服用6至12个月,或者在有复发风险的人群中服用长达2年,但许多人服用的时间更长。对长期服用抗抑郁药患者的长期调查显示,三分之一至一半的患者没有证据和理由继续服用抗抑郁药, 长期服用会增加副作用。
33项随机对照试验包括4995名参与者,他们服用了24周或更长时间的抗抑郁药。有13项研究突然停用了抗抑郁药,有18项研究停用了抗抑郁药,有4项研究也提供了心理治疗支持,还有一项研究是由于给全科医生的一封信指导停用了抗抑郁药。与大多数指南所建议的一样,大多数减药计划持续了4周或更短的时间。但最近英国皇家精神科医学院则建议,减药时间应更长,持续数月或数年。该团队回顾的研究也未能区分抑郁症复发的症状和任何药物戒断症状。研究人员指出,区分复发和戒断症状是一个真正的挑战,经常导致不适当的继续服用抗抑郁药物。Kendrick认为抗抑郁药的戒断症状很常见,可能会被误认为是潜在疾病的复发。经历戒断症状并不是病人复发的迹象,而是他们需要逐渐减少剂量,减少到更小的剂量,直到最终停止用药。这就需要更多的研究来确定患者戒断症状的发生率,还需要大型随机对照试验来测试不同的戒断策略。
我们确实需要更多的减药研究,尤其是在初级保健领域,因为大多数处方都是在初级保健领域开出的,然后才能得出更明确的结论。
原文出处
3、 Royal College of Psychiatrists. Stopping antidepressants. Sep 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抑郁药#
34
#Database#
30
已读,真是受益匪浅呀!
66
#ATA#
28
#抗抑郁#
35