The Anatomical Record:超声监测桡动脉——心脏病评估的新方法!
2017-04-16 枫丹白露 来宝网
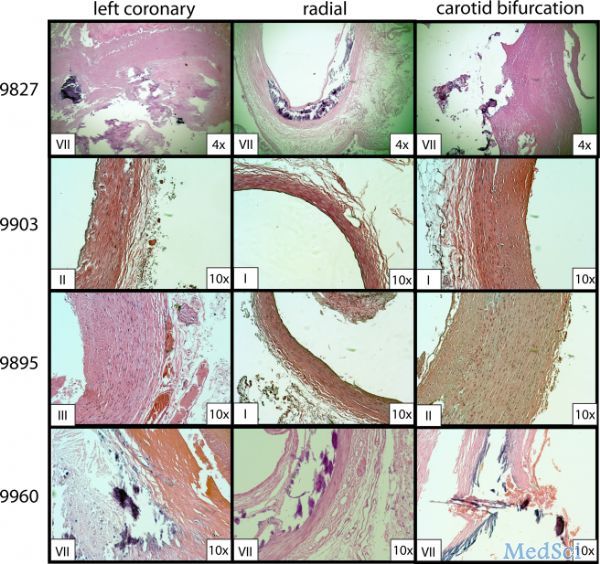
与传统的种族,年龄,性别和代谢特征的危险因素相比,动脉粥样硬化(通常被称为动脉硬化)长期以来被认为是冠状动脉疾病的强指标。与影响许多人的其他疾病不同,动脉粥样硬化目前没有简单的诊断或监测治疗反应的方法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ANA#
40
#Nat#
32
#新方法#
35
#anatomic#
49
学习过了,值得分享!!!
71
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了!
79
中医诊脉的科学理论!
61
#桡动脉#
28
,将桡动脉作为临床可及的位置进行超声波监测
68
桡动脉和冠状动脉一样都是中动脉,理论上是讲得通的;桡动脉的病变不是一个点,也许表现为不连续的某些段,如何监测还需标准化!
70