BJH: 首次使用抗 VWF 纳米抗体 caplacizumab 治疗妊娠期 iTTP
2021-12-23 MedSci原创 MedSci原创
免疫介导的血栓性血小板减少性紫癜 (iTTP) 是一种罕见的血栓性微血管病 (TMA),由针对金属蛋白酶 ADAMTS13 的自身抗体引起。随后超大血管性血友病因子 (VWF) 多聚体的积累诱导血小板
免疫介导的血栓性血小板减少性紫癜 (iTTP) 是一种罕见的血栓性微血管病 (TMA),由针对金属蛋白酶 ADAMTS13 的自身抗体引起。随后超大血管性血友病因子 (VWF) 多聚体的积累诱导血小板凝集和微血管血栓形成。怀孕会导致 iTTP 发作,也对医生提出了挑战,例如结合先兆子痫或 HELLP 综合征的特征,可能会增加孕产妇死亡率。
迄今为止,尚无关于使用 caplacizumab 治疗妊娠相关 iTTP 的数据。豚鼠的动物数据未报告不良反应。在这里,有研究报告了在 36 岁患有急性 iTTP 发作的孕妇中首次使用 caplacizumab的病例。
该患者在本次发作前 13 年被诊断出患有 iTTP。尽管进行了间歇性的利妥昔单抗治疗,但自三年前的最后一次发作以来,自身免疫活性持续存在,ADAMTS13 活性低于 10%,并且可检测到抗 ADAMTS13 自身抗体。患者拒绝进一步强化治疗,一年前停用免疫抑制药物。在随访期间,患者报告在 11 + 4 周估计胎龄 (EGA) 时怀孕。到那时,ADAMTS13 活性仍低于 10%,可检测到抗 ADAMTS13 抗体,表明急性 iTTP 和流产的风险增加。由于没有溶血活性或微血栓形成的迹象,开始使用糖皮质激素和硫唑嘌呤的免疫抑制药物治疗。在 17 + 1 周 EGA 时,患者出现食源性感染症状到我们医院就诊。实验室检查显示微血管病性溶血性贫血和血小板减少症(见表 I和图 1A)。超声显示胎儿发育正常,胎儿发育正常。除了硫唑嘌呤外,患者每天接受 PEX 和高剂量糖皮质激素。血小板计数在五天内恢复。两次额外的治疗后,PEX 被终止,但患者的病情立即恶化。到那时,胎儿仍然很重要,胎儿生长在正常的下限内(见图 1B)。值得注意的是,存在双侧切迹的子宫血管阻力增加,表明先兆子痫和严重宫内生长受限 (IUGR) 的风险增加。
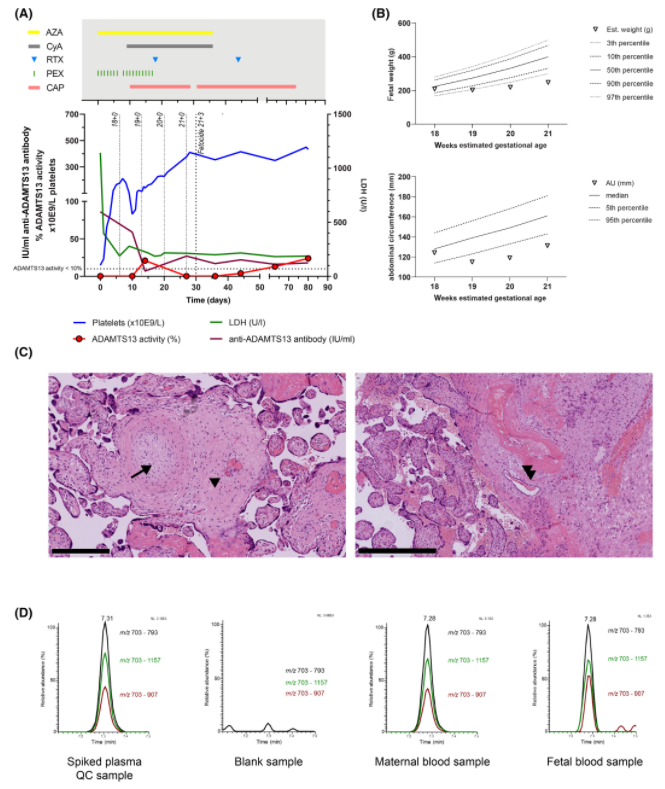
图::(A) 与疾病发作(第 0 天)和治疗相关的血小板、LDH 水平、ADAMTS13 活性和抗 ADAMTS13 抗体的时间线。36 天后停用环孢素 (CyA) 和硫唑嘌呤 (AZA)。请注意,第 14 天 ADAMTS13 活性的测量是在 PEX 上采样的,并没有报告患者的自身免疫水平。泼尼松龙(此处未显示)在疾病发作时以每天 100 毫克的最大剂量应用,并在两个月内小心减量。AZA,硫唑嘌呤;CyA,环孢素;RTX,利妥昔单抗;PEX,血浆置换;CAP,卡普拉珠单抗。(二)。以克为单位的胎儿体重和以毫米为单位的胎儿腹围作为与各自体重和腹围百分位数相关的胎儿生长参数。14,15X 轴表示以周为单位的估计胎龄 (EGA)。(C)。胎盘的组织病理学分析。左图显示由于胎儿血栓性血管病变导致的胎儿血管腔完全闭塞(箭头)和分隔(箭头)。右图显示蜕膜小动脉壁中的纤维蛋白沉积(双箭头),对应于先兆子痫中发现的动脉粥样硬化。苏木精和曙红染色,比例尺:250 µm。(四)。从 caplacizumab 获得的胰蛋白酶肽 T3 的特征前体/产物离子对的提取离子色谱图,来自加标血浆质量控制 (QC) 样品 500 ng/ml,空白血浆样品,患者的血浆样品给药后 15 小时收集10 mg caplacizumab 和在开始杀胎时收集的脐带血浆样本。
患者强调,即使在适应证外的适应症中,她也坚定地希望加强治疗。基于共同决策,环孢素、利妥昔单抗和 caplacizumab 作为标签外疗法给药。血小板计数在三天内恢复正常,但超声再次显示出明显的高子宫胎盘阻力,并伴有持续的双侧切迹。胎儿生长曲线进一步变平,这可能源于早发性胎盘功能不全。蛋白尿反弹至 647 mg/g 肌酐,加上新发高血压和升高的 sFlt-1/PlGF 比值,导致怀疑胎盘 iTTP 表现导致先兆子痫。一周后,诊断出严重的早发性IUGR,几乎没有间期生长,存在羊水过少和胎盘积水。鉴于胎儿预后不良,患者同意终止妊娠,以防止可能危及生命的 iTTP 和先兆子痫后遗症。
阴道分娩是有利的,并应患者的要求在分娩前通过心内注射钾进行宫内杀胎。征得患者知情同意后,采集胎盘组织、羊水和胎儿血样进行进一步分析。以防止可能危及生命的 iTTP 和先兆子痫后遗症。胎盘组织学显示绒毛发育迟缓、胎儿血管血栓形成、(母体)绒毛间血栓形成和与动脉粥样硬化相对应的蜕膜小动脉中的纤维蛋白沉积,如先兆子痫。然而,不存在小动脉壁肥大(先兆子痫的特征),表明慢性胎盘功能不全和胎儿血栓形成是严重早发性 IUGR 的主要原因。胎儿血管中的血栓是否表明胎儿 iTTP 表现仍然难以捉摸。之前已经描述了母体抗 ADAMTS13 抗体的经胎盘转移,但据我们所知,没有关于胎儿 iTTP 的报道。没有明显的出血并发症,特别是没有胎盘后血肿的迹象。
在 LC-HR-MS/MS 分析的帮助下,记录了 caplacizumab 的经胎盘转移(方法参见补充材料)。Caplacizumab 在羊水和胎儿血液中被定性鉴定,高于检测限,如图1D所示 。估计的药物浓度为 50 ng/ml。根据公布的药代动力学,母血中的估计浓度在预期范围内,因此高出五到十倍。caplacizumab 剂量是否不足以预防任何胎儿血栓形成,或者组织学证实的血栓形成是否由 pre-caplacizumab 微血栓形成导致仍然难以捉摸。
总之,患者的 caplacizumab 治疗似乎是安全有效的,三天内血小板计数迅速恢复正常。治疗迅速改善了母亲的状况,但可能应用得太晚而无法挽救胎儿的生命。
根据经验,对于未来妊娠早期 iTTP 的病例,可以吸取哪些教训?首先,iTTP 是一种影响母亲和胎儿的破坏性疾病,具有很高的不良后果风险。即使及时开始标准治疗——这对同一患者以前的急性 iTTP 发作有效——也不能预防 IUGR 和胎儿丢失。因此,在个别情况下,快速和坚定地开始 caplacizumab 治疗以预防血栓性微血管病似乎是合理的。其次,尽管 caplacizumab 可能会增加妊娠特异性出血并发症的风险,例如胎盘后血肿,但研究团队认为持续 TMA 造成的胎盘损伤与胎盘灌注受损对胎儿构成更大的风险。对于妊娠早期 iTTP 且流产风险高的前瞻性患者,他们将尽早使用 caplacizumab,并辅以糖皮质激素和 PEX。毫无疑问,这种治疗必须基于共同决策,经过彻底的风险收益讨论。一旦 TMA 消退,他们将停止 PEX 并继续使用 caplacizumab,具体取决于 ADAMTS13 活性、疾病严重程度和药物耐受性。
原始出处:
Kühne, L., Völker, L.A., Hagmann, H., Hägele, H., Osterholt, T., Eichenauer, D.A., Thomas, A., Breuer, J., Grüttner, B., Gottschalk, I., Kann, M., Benzing, T., Thevis, M., Müller, A.M. and Brinkkoetter, P.T. (2021), First use of the anti-VWF nanobody caplacizumab to treat iTTP in pregnancy. Br J Haematol. https://doi.org/10.1111/bjh.17833
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#CAP#
63
#Caplacizumab#
35
#mAb#
34
#TTP#
39
学习
59
#妊娠期#
29
#vWF#
26
#APL#
27