251th ACS:准确定位乳腺癌部位的新方法——口服药物
2016-03-21 QQduhp 译 MedSci原创
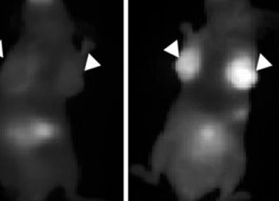
在第251届美国化学学会年会上,研究人员指出,通过口服药物可进行乳腺癌筛查,并能准确定位肿瘤细胞。乳腺癌是继皮肤癌后美国女性最常见的癌症。今年,约有超过246000名女性患有乳腺癌。女性乳腺癌患者数目居高不下,但自1989年以来该病发病率持续下降,研究人员认为在一定程度上归因于早期进行乳腺癌筛查的及时性。 乳腺癌筛查包括乳房x光检查,可使医生发现未能触及的乳腺癌肿块。 但许多人并不能通过这种方式发
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#口服药物#
40
#口服药#
36
#新方法#
37
想法不错,多途径检查,让病人选择
109
口服药片可区分肿瘤组织是良性还是恶性?这个难!
131
口服药(含有荧光显像剂),服用这种药片后,它们可以与肿瘤细胞或肿瘤特异性血管细胞紧密贴附在一起。然后通过红外光照射,显像剂会发出荧光,使得癌变肿瘤显像。
164
#ACS#
42
好创意
67
有点意思
118
这是真的?
89