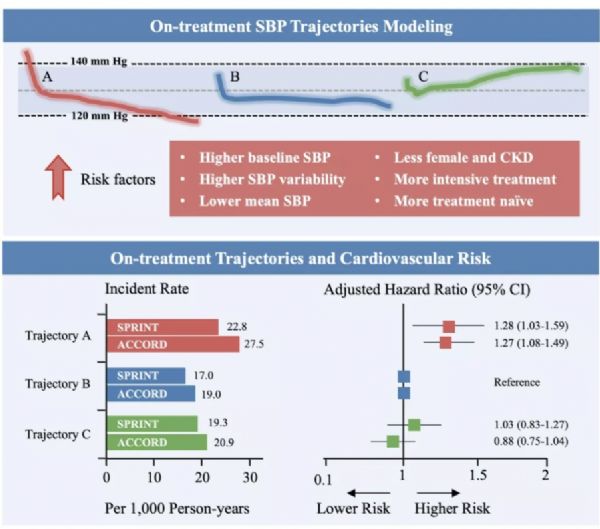
AHA中国之声:降压治疗的收缩压轨迹与心血管疾病风险:不同试验中的相似模式
2019-11-18 国际循环编辑部 国际循环
11月16~18日,由美国心脏协会(AHA)主办的2019科学年会在美国费城召开。中山大学附属第一医院心血管内科庄晓东博士在大会上汇报了《Data-driven Trajectories of On-treatment Systolic Blood Pressure and Cardiovascular Risk in SPRINT and ACCORD:Similar Pattern in Di

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#收缩压#
48
#AHA#
48
#降压#
39
#降压治疗#
56
#疾病风险#
48
#血管疾病#
38