NEJM:下肢无力与感觉迟钝,最后诊断竟然是……?
2017-07-03 月下荷花 肿瘤资讯
MEJM的每期病例,其经典性不必赘述,看看这次又是什么样的离奇病例以及如何抽丝剥茧?
MEJM的每期病例,其经典性不必赘述,看看这次又是什么样的离奇病例以及如何抽丝剥茧?
临床表现
53岁女性,因进展性不对称性下肢无力及感觉迟钝入院。4个月前出现左足侧面感觉迟钝,2天后累及足趾和足中部,自述有慢性腰痛,向臀部放散,疼痛逐渐加重,无下肢疼痛、发热、体重减轻和尿便改变。家庭医生检查发现左足趾和左前足触觉和痛觉消失,ESR、B12、糖化血红蛋白、促甲状腺素正常。
5天后感觉迟钝向上进展至近端足部、踝以及小腿侧面,无痛。颅神经检查正常,左侧足趾屈展、左踝跖屈背屈、左足内外翻和左膝屈曲均为4+/5,左大拇趾的振动感觉明显下降,左足触觉和痛觉减弱,左侧跖反射消失。7天后神经传导检查发现感觉与运动反应均正常,左侧比目鱼肌Hoffman反射缺如,右侧正常;左下肢肌电图显示募集相消失,L5肌节远端和近端肌肉的多相运动单位电位消失。
脊髓增强MRI见间盘突出、黄韧带增生、椎间关节病,左侧L4-5神经孔中度狭窄,双侧L5-S1神经孔中重度狭窄,L3-S1神经根增厚、成簇、强化(图1)。脑脊液(CSF)分析无寡克隆条带,多形性淋巴细胞增多,免疫表型未提示单克隆细胞亚群。
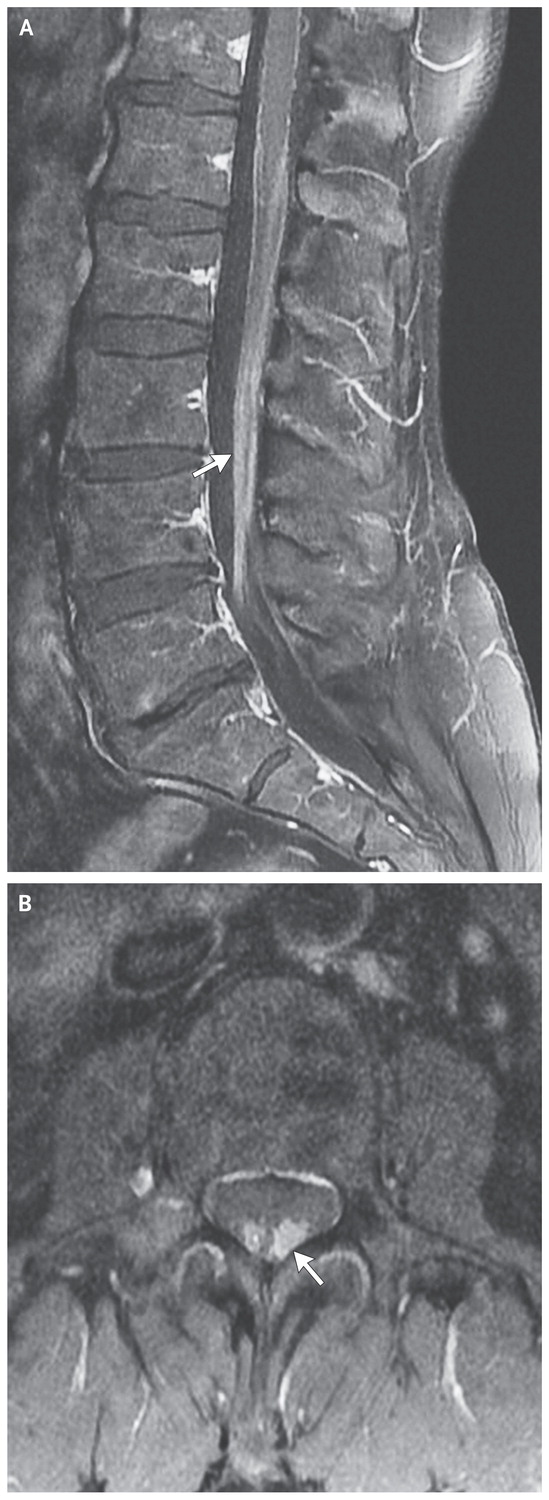
图1 诊断前3个月的脊髓MRI,箭头处为椎管内成簇、增厚、强化的马尾神经根
暂诊断为慢性炎症性脱髓鞘多发神经病,免疫球蛋白治疗后左下肢症状无改善,同时右下肢也出现无力感及感觉迟钝,并向躯干进展。患者曾有跌倒并开始使用拐杖,最后不得不使用轮椅,当患者不能由坐位站起时再次就诊,此时伴有尿便失禁。
患者1年半前诊断类风湿关节炎,甲氨喋呤+强的松治疗,7个月前干扰素γ释放检查阴性,加用依那西普;肺CT见双下肺不足1厘米小结节,4年间无变化;胃食管返流、子宫平滑肌瘤和轻型地中海贫血病史;1个月前钼靶检查正常;使用药物包括奥美拉唑、甲氨喋呤、强的松、叶酸、加巴喷汀、度洛西汀,因怀疑症状与依那西普有关而停用。吸烟史,18包年,不饮酒,其姐患多发性硬化,无癌症家族史。
体温36.3°C,血压168/78 mm Hg,脉搏90次/分,血氧饱合度100%,双下肢肌力4/5,双足趾至膝上的振动感觉和温度明显下降,膝肌腱深反射1+、对称,比目鱼肌腱深反射消失,无助力时不能站立,2个质硬、无痛皮下结节(约1厘米)位于左下颌下区。肝肾功能、电解质、血糖、CRP正常,小细胞性贫血,HIV、梅毒阴性,血管紧张素转换酶阴性。
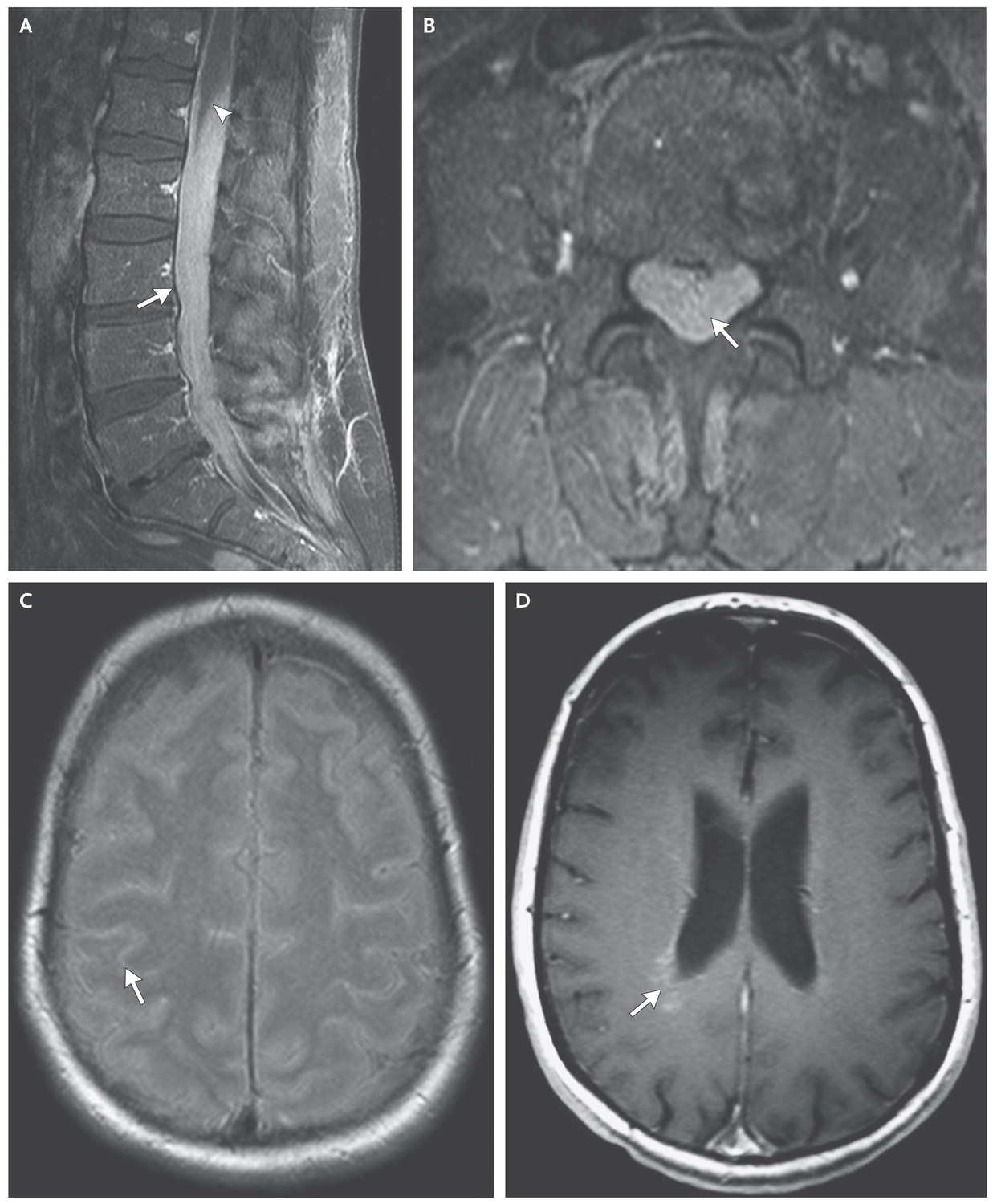
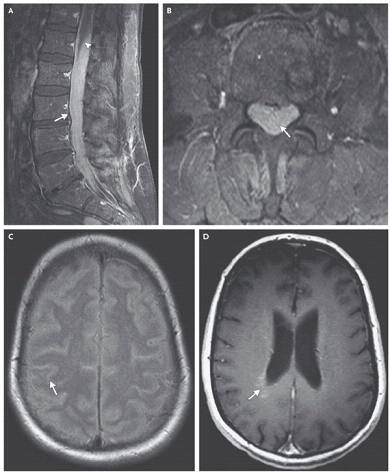
再次脊髓增强MRI(图2A和2B)见脊髓内弥漫、不规则、异常高密度影,自T10下缘到骶椎,神经根明显增厚强化。头增强MRI(图2C和2D)见双侧脑沟弥漫高密度影,无脑膜强化。双侧脑室周围片状、界限不清病灶伴强化。胸部CT同前。重复神经传导检查见不对称的感觉和运动反应振幅减低,左侧重于右侧,无脱髓鞘证据。电生理检查见T8双侧椎旁肌肉、臀大肌、阔筋膜张肌、腓肠肌和右侧胫前肌异常自发活性,所有双下肢肌肉的运动单位电位募集相弥漫性降低。
再次脑脊液检查蛋白4620 mg/dl,糖<2 mg/dl,多形性、体积增大的淋巴细胞增多,免疫表型提示B细胞,胞浆表达κ和λ轻链。活检结节组织不足以进行病理评估,三次痰抗酸菌检查阴性。患者出现尿潴留、直肠无张力、鞍区感觉迟钝。
图2 入院时的脊髓和头部MRI,A和B显示椎管内成簇、增厚、强化的马尾神经根进展(有尾箭头),伴硬膜囊完全消失,对胸下段脊髓和圆椎的肿块压迫效应(无尾箭头),C显示脑沟强化,D显示脑室周围白质片状、边界不清的强化影,伴侧脑室增大
鉴别诊断
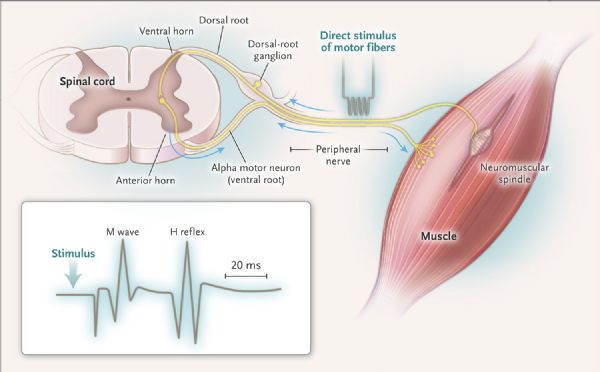
患者远端反射减弱或消失,疾病定位于外周神经系统。累及外周神经导致肌无力的疾病包括肌纤维疾病、神经肌肉接头疾病、神经疾病或前角细胞疾病。患者主要表现为感觉症状,提示为神经疾病,多神经炎表现为多灶性和非对称性,受累神经区域功能异常,与感染、炎症、癌症和胶原血管病相关;有时神经根和背根神经节区域的神经束损伤后也会出现双侧非对称性感觉和运动障碍(图3)。
图3 外周神经系统解剖与反射
该患初始表现为背痛和远端单侧肢体麻木无力感,主要由L5和S1肌节支配的肌肉受累所致。鉴别诊断包括多神经根病、腰骶神经丛病变和坐骨神经病。神经传导检查显示患肢缺少H反射,腓感觉神经反应正常(图3),提示损伤定位神经根,神经传导研究显示下肢感觉反应未受累,不支持神经丛或神经受累,肌电图也证实L5肌节支配肌肉受累。患者的症状在一个区域内不断进展,考虑为局部结构性改变压迫周围神经束所致。临床上双下肢感觉和运动功能异常,最终出现鞍区感觉迟钝、尿潴留、便秘,这些均提示累及骶下神经根。
根据MRI表现以及病情进展特点,可以推断疾病累多个腰骶神经根并对圆椎产生压迫,不清楚是否累及脊髓,T10段以下脊髓的无强化异常信号提示为压迫导致的水肿或血管充血,也可能有轻度脑膜受累。
第二次电生理检查显示病情明显恶化,腓和胫神经运动反应下降加重,L5-S1水平多块肌肉急性损伤;除了腰骶神经根受累表现外,T8水平脊柱旁肌肉异常,提示胸神经根或前角细胞受累;逐渐出现的下肢感觉反应明显减退,提示疾病累及背根神经节或神经丛或下肢外周神经。因此该患诊断必需能同时解释双侧多个腰骶神经根、胸段神经根和近端腰骶神经从受累。
除了解剖定位、图像改变、CSF异常和电生理结果,其它需要考虑的因素包括肺结节、类风湿关节炎病史、甲氨喋呤+强的松+依那西普免疫调节治疗。腰骶髓MRI显示增厚、成簇、强化神经根,改变为非特异性,可以是炎症、感染和癌症;CSF中糖明显下降,蛋白明显增高,淋巴细胞明显增多,可见于结核、结节病、癌性、淋巴瘤性或白血病性脑膜炎,不过CSF中的淋巴细胞无法分类,重复CSF检查也未能发现癌细胞或是单克隆改变;类风湿关节炎和免疫调节治疗病史可能增加淋巴瘤、结核、结节病、癌症可能,但因果关系并不十分明确。
1.结节病
患者肺内有结节,因此要注意结节病可能。但如下几方面不符合,包括血管紧张素转换酶阴性,CSF中蛋白和细胞增加远超过结节病,患者有明显的感觉迟钝却无疼痛,而结节病累及外周神经系统虽然很罕见,如果存在则有典型疼痛,明显超过无力感和感觉迟钝。
2.结核
免疫抑制且有肺结节,因此高度注意结核,不过患者未生活在结核流行区,依那西普治疗前干扰素γ释放检查阴性,痰抗酸菌阴性,不支持结核,CSF改变的严重程度也超过了结核性脑膜炎,无头痛症状在结核性脑膜炎中很少见。
3.癌症
疾病快速进展提示侵袭性浸润过程,癌症或淋巴瘤转移导致的癌性脑膜炎也有可能。系列肺部CT显示肺结节稳定,不支持肺癌转移;腹盆腔检查未发现其它可疑损害;乳腺钼靶正常;外周血改变不明显可除外白血病。所以该患最可能诊断是孤立性淋巴瘤性脑膜炎,此类患者多数有全身疾病表现,如发热、体重减轻和盗汗,该患无上述表现,提示疾病相对局限。
4.总结
该患诊断需要更多证据,最恰当的策略就是组织活检,该患有几处可供活检的部位:脑膜、外周神经或神经根。神经根活检虽然困难,但诊断率可能最高,因为多数症状集中于此。
神经外科治疗
L1–L2水平椎板切除,微切珠网膜和软脑膜,暴露神经根,发现硬脑膜张力增高,蛛网膜增厚,神经根增厚、成簇、充血、血管增生。从神经根主干切取一分支进行病理评估。
病理讨论
病理提示神经内细胞明显增多(图4A),一种是看起来正常的淋巴细胞,细胞核小而圆,染色质深染,另一种是大的细胞,核膜不规则,开放染色质和突出的核仁(图4A),散在分裂相。大细胞的外表是典型的恶性淋巴细胞,免疫组化显示恶性细胞并未形成明确肿块,而是弥散性浸润神经纤维(图4B),CD45阳性,CD20(图4C)阳性,Ki-67(图4D)显示分裂细胞明显增多,支持恶性诊断。根据这些结果诊断为弥漫大B细胞淋巴瘤,其浸润性生长模式与弥漫性神经浸润相符。
图4 神经根活检 A为二种形态的淋巴细胞,箭头处为恶性淋巴细胞伴有丝分裂,B显示恶性细胞向神经纤维浸润,C CD20阳性,D Ki67显示肿瘤的高度增殖性。
治疗讨论
进一步检查未发现其它部位受累,按照孤立原发中枢神经系统淋巴瘤,给予高剂量化疗甲氨喋呤+利妥昔单抗+替莫唑胺。10次甲氨喋呤治疗后,MRI 显示病情改善,获CR,下肢肌力和感觉改善。自体干细胞移植顺利,患者病情持续改善,移植后1年MRI未提示疾病复发。
点评:淋巴瘤的改变千奇百怪,给力的神经外科活检、患者良好的依从性为最终诊断添上了最重要的一份证据。
原始出处:
William S. David, Michael P. Bowley, et al. Case 19-2017 — A 53-Year-Old Woman with Leg Numbness and Weakness. N Engl J Med 2017; 376:2471-2481June 22, 2017DOI: 10.1056/NEJMcpc1701762
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#下肢无力#
49
淋巴瘤的表现真是千奇百怪!!!
4
学习
93
谢谢分享
89
学习了谢谢分享
88
学习了分享了
71
学习了,谢谢分享
31
好东西学习了!
0