J Clin Invest:创新性细胞疗法有望治疗对当前免疫疗法并无反应的癌症患者
2019-11-04 佚名 细胞
在当今精准化治疗癌症的时代,研究人员正在不断努力开发新型个体化疗法来释放机体免疫系统的功能从而有效治疗多种疾病;尽管相关研究取得了很大的成果,但研究者仍然需要进行大量工作来更好地预测哪些患者能因治疗而获益,同时将这些治疗效益扩展到更多患者及肿瘤类型中。
在当今精准化治疗癌症的时代,研究人员正在不断努力开发新型个体化疗法来释放机体免疫系统的功能从而有效治疗多种疾病;尽管相关研究取得了很大的成果,但研究者仍然需要进行大量工作来更好地预测哪些患者能因治疗而获益,同时将这些治疗效益扩展到更多患者及肿瘤类型中。
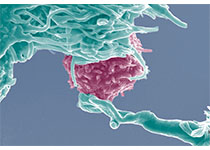
近日,一项刊登在国际杂志Journal of Clinical Investigation上的研究报告中,来自Vall d'Hebron肿瘤研究所的科学家们通过研究开发出了一种新型疗法,其能能有效治疗对当前免疫疗法并无反应的癌症患者。更具体地说,那些携带低突变负担(所谓的“冷”肿瘤)的胃肠道肿瘤患者已经成为了当前免疫疗法的挑战,基于能识别新抗原的杀伤性T细胞给药疗法目前已在少数“冷”肿瘤患者机体中展现出了潜在的抗肿瘤活性。
本文研究有望帮助研究人员开发新型疗法来治疗对已批准的癌症疗法并无反应的转移性癌症患者;此外,研究者还描述了一种微创、基于血液的新方法来识别、测定并追踪抵御恶性胃肠道癌症所表达的新抗原(肿瘤抗原),这些癌症包括胰腺癌、胃食管癌、胆管癌和结直肠癌等。研究者Alena Gros指出,虽然我们并不期待能够在低突变负担“冷”肿瘤患者机体血液中找到杀伤性T淋巴细胞,但如今研究表明,我们能够识别并选择血液中的这些细胞,来通过液体活检技术开发新型个体化细胞疗法。
目前研究人员正在通过联合研究来寻找新型制剂,从而抑制免疫系统的检查点调节、解析癌症耐药机制及患者对疗法的反应,研究者的主要目标就是开发出新型细胞疗法来有效治疗癌症患者。最后研究者表示,本文研究或能促进他们从癌症患者血液中寻找新抗原特异性的T淋巴细胞,从而为寻找或开发新型抗癌个体化疗法提供新的思路和希望。
原始出处:
Alena Gros,Eric Tran,Maria R. Parkhurst, et al. Recognition of human gastrointestinal cancer neoantigens by circulating PD-1+ lymphocytes, Journal of Clinical Investigation (2019). DOI:10.1172/JCI127967
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#EST#
35
#创新#
39
#癌症患者#
35