JACC:严重COVID-19的ACHD特异性危险因素
2021-03-30 “心关注”微信号 “心关注”微信号
强调在评估ACHD患者严重COVID-19的潜在风险时,我们不能忽视非基于ACHD的风险因素,因为它们可能导致更严重的COVID-19和死亡,尤其是与本研究所见的晚期生理阶段相结合时。
在全球严重急性呼吸综合征冠状病毒-2(SARS-CoV-2)健康危机爆发之初,从业者焦急地观察并试图理解这种新病毒将如何影响患者。在中国武汉报告的第一例病例的1个月内,我们开始了解到冠状病毒病-2019(COVID-19)可能会扩展到肺系统以外,在许多情况下会导致以血管炎症、心肌炎和心律失常为特征的急性心脏损伤。更糟糕的是,随后的证据表明,有潜在心血管疾病的患者患严重COVID-19和死亡的风险更高。我们这些在成人先天性心脏病(ACHD)社区的人开始为我们的病人担心;这个群体已经克服了难以置信的医疗、手术和心理社会负担,因为在他们年轻的生活中存在先天性心脏病(CHD)。
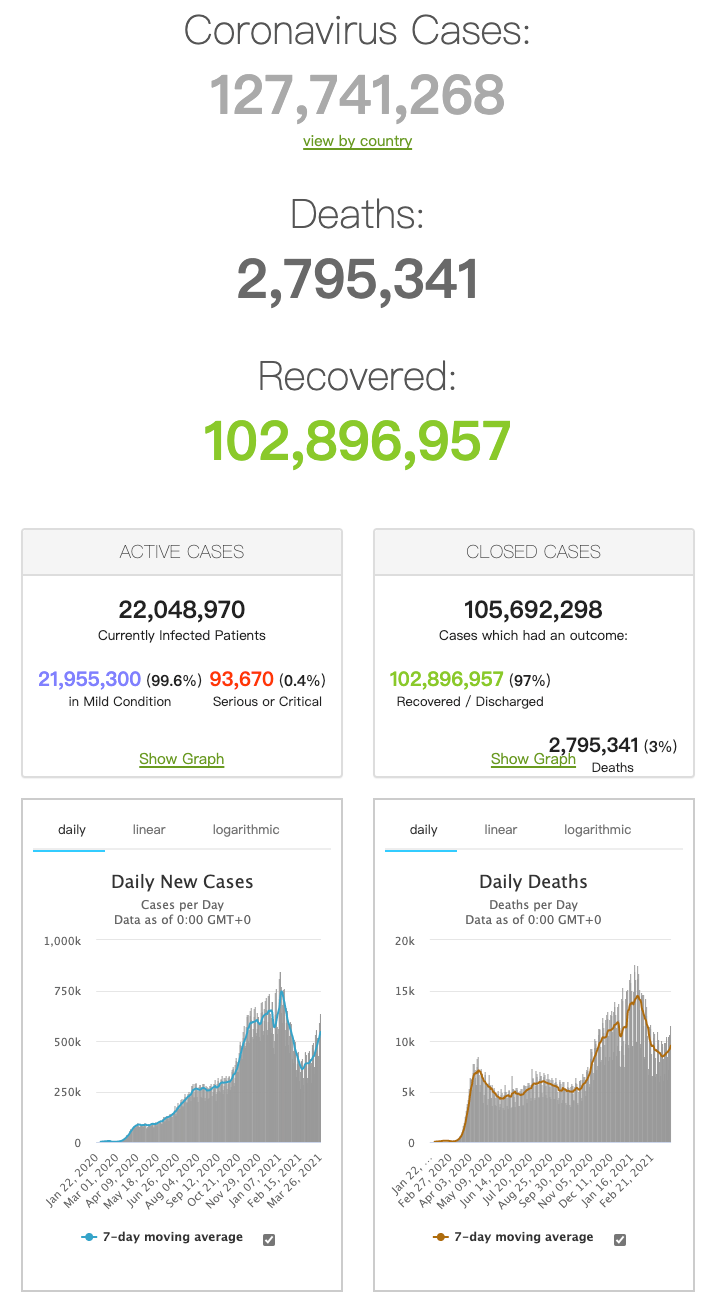
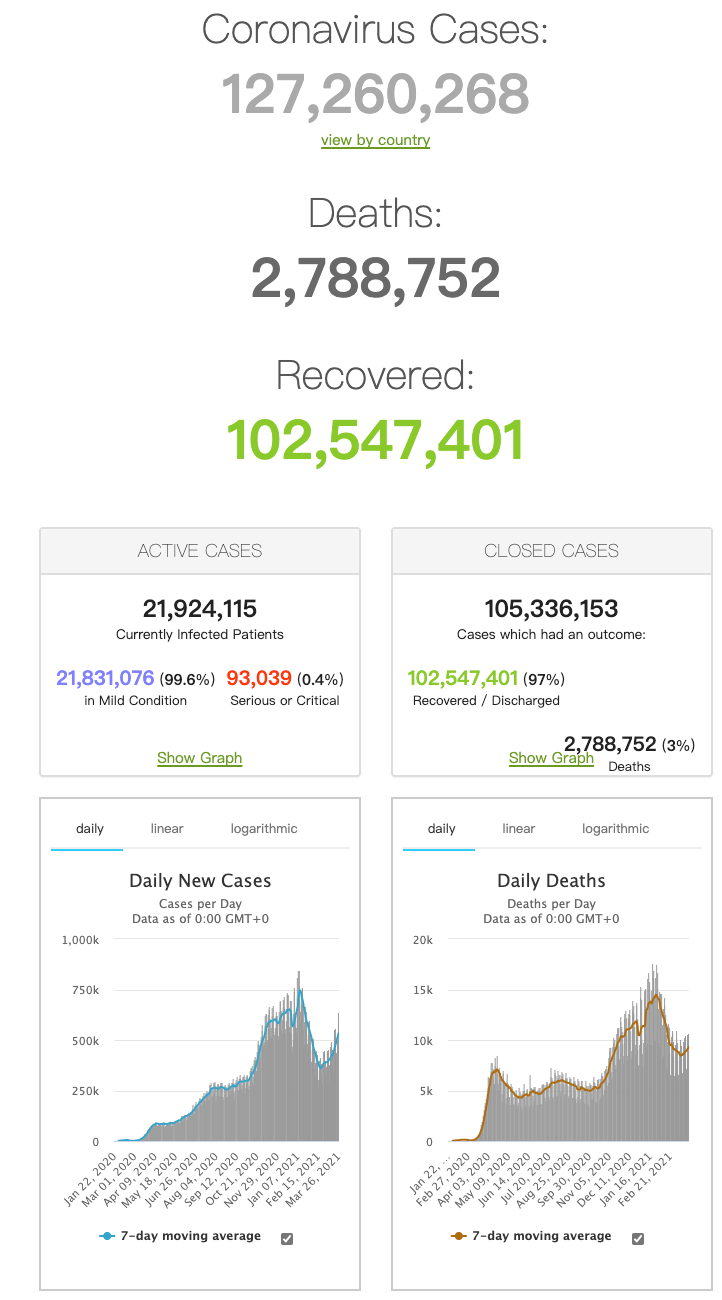
在过去的一年中,我们依赖于小型研究,并推断出在ACHD中COVID-19的潜在风险,通常希望我们基于对该疾病的最小集体和轶事个人经验是正确的。因此,在本期杂志中,Broberg等人对来自北美、南美、欧洲和西亚58个中心的1044例ACHD患者的COVID-19结果进行了大规模的回顾性研究,这是及时的。本研究的主要目的是确定是否存在与以下因素相关的危险因素:1)伴有COVID-19的ACHD患者的死亡率增加;2)重症监护病房(ICU)入院、气管插管、急性呼吸窘迫综合征和/或肾脏替代治疗的需要所定义的严重感染。
研究者因纳入大量的COVID-19和ACHD患者而受到赞扬。共有907名患者(87%)在实验室确认了COVID-19(聚合酶链反应或抗体阳性)。ACHD基于结果的研究的挑战之一是如何解释显着的解剖异质性,这会使整个疾病谱中的结果真正准确的可能性复杂化。为了克服这一问题,研究人员根据最新的美国指南:简单、中度或严重复杂疾病[11],将冠心病的解剖结构按最复杂的心脏缺陷分类,每一项只统计一次。根据患者的基本生理阶段(A、B、C、D),将患者分为亚组,以评估冠心病对功能的影响[11]。最后,对基于年龄的三分位数(18至27岁、28至40岁、41岁或以上)进行第三级分析,试图确定年龄本身是否影响ACHD人群的COVID-19结果。
总共有179例(17%)入院(重症监护病房67例[6.4%])和24例COVID-19相关的住院死亡,导致总病死率(在受试者中)为2.5%(95%可信区间:1.5%至3.6%),与非ACHD队列中的报告相似[12]。在死亡组中,近一半是紫绀型,约17%的患者有肺动脉高压(PAH)而无紫绀型或既往有心力衰竭病史。有趣的是,相当数量(n=7;30%)的死亡患者有简单解剖复杂的病变,然而正如研究者所说,由于非冠心病的原因,包括糖尿病、肥胖和老年人,仍然存在严重COVID-19的高风险。单纯病变和生理期A和/或B疾病患者没有死亡,这意味着单纯病变患者也有晚期生理期(C和/或D)。因此,强调在评估ACHD患者严重COVID-19的潜在风险时,我们不能忽视非基于ACHD的风险因素,因为它们可能导致更严重的COVID-19和死亡,尤其是与本研究所见的晚期生理阶段相结合时。

Corresponding Author
COVID-19 in Adults With Congenital Heart Disease
JACC. 2021 Apr, 77 (13) 1644–1655
Background
成人先天性心脏病(CHD)被认为是新的冠状病毒病-19(COVID-19)死亡率或其他并发症的潜在高风险。
Objective
本研究旨在确定COVID-19在成人冠心病患者中的影响,并确定与不良结局相关的危险因素。

Methods
包括全球CHD中心的成人(18岁或18岁以上)以及经证实或临床怀疑的COVID-19。数据收集包括解剖诊断和后续干预、合并症、药物、超声心动图发现、症状、病程和结果。确定死亡或严重感染的预测因子。
Results
来自58个成人冠心病中心的1044名感染者(年龄:35.1±13.0岁;范围18-86岁;51%为女性),其中87%的人有实验室确诊的冠状病毒感染。队列包括118例(11%)单心室和/或Fontan生理的患者,87例(8%)紫绀患者和73例(7%)肺动脉高压患者。共有24例COVID相关死亡(病例/病死率:2.3%;95%可信区间:1.4%至3.2%)。与死亡相关的因素包括男性、糖尿病、紫绀、肺动脉高压、肾功能不全和曾因心力衰竭入院。生理分期越差,死亡率越高(p=0.001),而解剖复杂或缺损组则不相关。
Conclusions
冠心病成人COVID-19死亡率与一般人群相当。最脆弱的患者是那些生理阶段较差的患者,如紫绀和肺动脉高压,而解剖结构的复杂性似乎不能预测感染的严重程度。
可以说,这项研究最重要的发现之一是解剖结构的复杂性本身并不能预示COVID-19的预后更差;然而,必须承认,护理方面的历史进展可能会影响这一人群目前基于年龄的异质性,并可能混淆这一结果。相反,这个故事的一个关键部分展开了——晚期生理阶段(C期和D期)患者使用COVID-19的死亡风险最高(分别为3.9%和7.9%,而a期和B期分别为0%和1.1%)。特别是,发现与严重COVID-19和死亡相关的ACHD特异性危险因素包括紫绀、静息缺氧、房性心律失常、肾(终末器官)功能障碍和临床上重要的心力衰竭(入院)。这些临床特征在指定生理阶段时被常规评估,因此,开始识别出患有乙酰胆碱酯酶D的患者,这些患者有较高的严重COVID-19的风险,可能是由于其潜在的CHD(所谓的乙酰胆碱酯酶D特异性危险因素)。随着疫苗接种战略的发展和保护高危人群的优先事项开始出现,这一点越来越重要。
在美国,疾病控制和预防中心(CDC)的免疫实践咨询委员会(ACIP)为COVID-19疫苗的分发提出了分配建议。该建议优先考虑高风险接触COVID-19的人群,如卫生保健人员和长期护理机构的居民,以及严重疾病的高风险人群,主要是老年人群。然而,阶段推荐系统(1a,1b,1c,2)还不清楚应该评估哪些心血管因素来评估严重COVID-19的个体风险。特别是,这一点在1c期分类中起到了作用,在1c期分类中,建议“16-64岁患有高风险疾病的人”。在最初的建议中,以下情况会增加严重COVID-19的风险:“癌症、慢性肾脏疾病、慢性阻塞性肺疾病、心脏病如心力衰竭、冠状动脉疾病或心肌病;实体器官移植导致的免疫损害状态(免疫系统减弱);肥胖(体重指数[BMI]>30 kg/m2,但<40 kg/m2);严重肥胖(BMI≥40 kg/m2);镰状细胞病、吸烟;2型糖尿病和妊娠”。国家和地方的做法使疫苗分配问题更加复杂,这些做法可能不直接遵循疾病预防控制中心提出的建议,而且在许多情况下,提到“先天性疾病”可能有资格提前接种疫苗。

图1. ACHD患者严重COVID-19的危险因素分析
为了评估成人先天性心脏病(ACHD)严重冠状病毒病-2019(COVID-19)的风险因素,重要的是评估非ACHD风险因素,如美国疾病控制和预防中心等组织提出的,以及与ACHD相关的风险因素(即生理阶段C和D)。在这项研究中,新的乙酰胆碱酯酶特异性危险因素(红框)被识别出来,在对严重疾病的个体风险进行全面评估时应予以考虑。
*心脏病,如心力衰竭、冠心病或心肌病。BMI=体重指数;NYHA=纽约心脏协会;O2=氧气。
ACIP对有潜在心脏病的人提出了广泛的建议,这很可能是有意的,因为这个术语包含了广泛的疾病和不同的生理和功能影响。然而,作为一个社区的乙酰胆碱酯酶从业人员,“可以踢”给我们,以帮助确切地确定哪些病人可能有风险严重COVID-19。尽管研究人员并未着手确定哪些患有乙酰胆碱酯酶的患者可能从早期疫苗接种中获益,但这是我们头脑中最重要的问题之一,因为我们的目标是以一种道德责任感和数据驱动的方式保护高风险群体。当我们考虑如何在SARS-CoV-2大流行期间对患有ACHD的患者进行风险分层时,所提供的数据突出了几个要点:1)我们不能忘记非ACHD-COVID-19风险因素,如糖尿病、年龄和体重指数,因为有相当一部分患有单纯CHD和高级生理学分级的ACHD患者已经屈服于具有这些危险因素的COVID-19;2)我们需要开始评估研究人员概述的ACHD特定危险因素[10],这些因素似乎与严重的COVID-19有关,包括紫绀,临床上重要的心力衰竭、静息缺氧、生理晚期和多环芳烃病史(图1)。由于这些因素与病死率相关,考虑优先考虑具有≥1个ACHD特异性严重COVID-19危险因素的ACHD患者可能是合理的。特别是在美国,这将明确ACIP建议1c期ACHD患者子集的资格。然而,随着大流行的持续,科学数据不断发展,我们对特殊人群中这种新疾病的了解也越来越全面。我们很可能期待对这一队列以及EPOCH(欧洲先天性心脏病前瞻性结果研究合作)COVID-19跟踪项目[9]的进一步分析,这两个项目都将继续影响我们如何评估风险、治疗管理和保护ACHD患者免受COVID-19的影响。
原始出处:
Broberg C.S., Kovacs A.H., Sadeghi S., et al. ACHD-Specific Risk Factors for Severe COVID-19. J Am Coll Cardiol 2021;77:1644-1655.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特异性#
28
#JACC#
24
#ACC#
24
#CHD#
38
#ACHD#
31
好文
82
很好
78
好文章!
78