Lancet Oncology:癌症患者的希望之光,万能靶向药再出手,可降低78%疾病进展与死亡危险!
2021-07-13 生物探索 生物探索
卡博替尼的3期临床试验结果将为无可用治疗标准的放射性碘难治性DTC患者提供一种新的治疗选择。
卡博替尼(cabozantinib),一款多靶点广谱抗癌药,能抑制包括MET、VEGFR2、RET、AXL等在内的多个靶点,目前已经在肾癌、甲状腺癌、肝癌、软组织肉瘤、非小细胞肺癌、前列腺癌、乳腺癌、卵巢癌等多种实体瘤中证实了较好的治疗效果,对于骨转移的控制效果尤其突出,也因此被称为“靶向药中的万金油”、“抗癌神药”等。
近日,美国制药公司Exelixis在 The Lancet Oncology 上发表了关于卡博替尼的最新临床试验进展,用于治疗分化型甲状腺癌(differentiated thyroid cancer,DTC),其题目为“Cabozantinib for radioiodine-refractory differentiated thyroid cancer (COSMIC-311): a randomised, double-blind, placebo-controlled, phase 3 trial ”。临床试验结果显示,卡博替尼能够显着延长先前接受VEGFR靶向治疗的放射性碘难治性DTC患者的无进展生存期,同时能够显着降低疾病进展或死亡风险。
https://doi.org/10.1016/S1470-2045(21)00332-6
甲状腺癌向来被称为“温柔的癌症”,分化型甲状腺癌占甲状腺癌的90–95%,主要包括乳头状癌和滤泡状癌。此类癌症治疗策略灵活,若进行积极监测、手术和放射性碘治疗,患者的预后一般相对良好,但是,仍有高达15%的患者在治疗期内会发展为放射性碘难治性转移性疾病,预后较差。这类患者在接受索拉非尼(sorafenib)或乐伐替尼(lenvatinib)的药物治疗后,会产生抗药性,从而加重病情导致死亡,其中位总生存期不超过5年,并且目前尚无有效的治疗护理标准。因此,如何满足这一群体的医疗需求显得尤为迫切。
此次名为COSMIC-311的临床试验,是一项全球性、多中心、随机、双盲、安慰剂对照的3期试验,用于评估卡博替尼对先前接受过VEGFR靶向治疗的放射性碘难治性DTC患者的疗效与安全性。
来自25个国家164家诊所的187位患者参与其中,随机按照2:1比例分配接受卡博替尼(n=125)或安慰剂(n=62),他们中位年龄为66岁,55%的患者为女性,已经被确诊为分化型甲状腺癌,并在此次试验前接受过索拉非尼和乐伐替尼的治疗。
试验以前100名随机分配患者的客观缓解率和所有随机分配患者的无进展生存率为主要终点,其中,客观缓解率数据以客观缓解率意向治疗人群(Objective response rate intention-to-treat population,OITT)为主,无进展生存率以意向治疗人群(Intention-to-treat population,ITT)为主,达到以上任一终点即可表明卡博替尼的治疗优于安慰剂。
临床试验数据结果显示,在中期分析中, ITT人群达到了无进展生存期的主要终点,卡博替尼与安慰剂相比,疾病进展或死亡的风险显着降低了78%。在ITT人群中,接受卡博替尼的患者有76%的目标病变缩小,而接受安慰剂的患者仅有29%的目标病变缩小;两个治疗组均未达到中位总生存率,但卡博替尼仍然显着改善了总生存期,死亡风险显着降低46%,其6个月总生存率更高,达到了85% 。
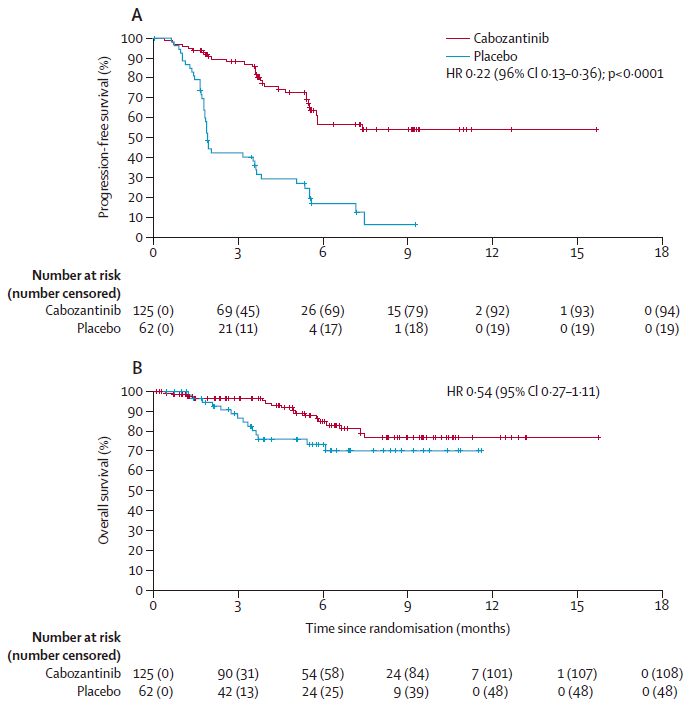
ITT人群卡博替尼组与安慰剂组的无进展生存率(A)与总生存率(B)对比
在安全性方面,卡博替尼组因治疗引起的不良事件而停药的比率为5%,并有71名受试者出现了3级或4级不良事件,主要病症为手足综合征、高血压、疲劳虚弱等。
早在2021年2月份,卡博替尼就已经被美国FDA授予突破性疗法认定,用于治疗放射性碘难治性分化型甲状腺癌。如今,甲状腺癌的发展呈上升趋势,2021年,美国将产生大约44000例甲状腺癌确诊病例,其中近四分之三的病例将会是女性,且诊断年龄趋于年轻化,而在国内,甲状腺癌的最新发病率是14.6/10万,而世界平均发病率为6.7/10万。因此,此次临床试验结果将为这一癌症患者群体带来福音,为无可用治疗标准的放射性碘难治性DTC患者提供一种新的治疗选择。
原始出处:
Marcia S Brose, et al. Cabozantinib for radioiodine-refractory differentiated thyroid cancer (COSMIC-311): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet Oncology, 2021. DOI:https://doi.org/10.1016/S1470-2045(21)00332-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncology#
38
#Oncol#
38
#Lancet#
34
#疾病进展#
32
#癌症患者#
39
#死亡危险#
26
顶刊就是不一样,质量很高,内容精彩!学到很多
59
谢谢梅斯分享这么多精彩信息
49