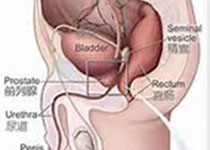
Prostate Cancer P D:针对性治疗男性穿刺活检中的细胞周期进程(CCP)评分在预后中的应用分析
2019-07-17 AlexYang MedSci原创
在局部前列腺癌男性患者中,准确的风险分层能够帮助指导进行合适的治疗选择。最近,有研究人员在一个大的、汇总分析中评估了针对性治疗的前列腺癌男性中,分子细胞周期进程(CCP)评分和组合细胞周期临床风险(CCR)评分预测10年恶化为转移性疾病风险的能力。汇总分析包括了1062名患者。研究发现,在调整了CAPRA(前列腺癌风险评估)、治疗类型和群体后的多变量分析中,CCP评分与10年转移疾病风险强烈相关(
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#穿刺活检#
0
#活检#
34
#细胞周期#
33
#穿刺#
27
#ROS#
32
#PRO#
27
#Prostate Ca#
26