PRS:提高治疗效率和患者生活质量,针对烧伤后神经疼痛成因来镇痛!
2021-03-15 MedSci原创 MedSci原创
该研究提出了由直接神经损伤、神经压迫、电损伤和继发于全身损伤的神经功能障碍组成的分类方法,可指导患者的治疗和研究方法,以改善烧伤相关神经疼痛的疼痛结局。
烧伤患者会有与损伤本身相关的急性疼痛、与清创术和植入术相关的急性疼痛,可能还有愈合阶段的疼痛。烧伤医生精通适当采取药物治疗缓解急性疼痛。但对于烧伤患者出院时有慢性神经性疼痛的机制,人们不太了解,也不太清楚。这种慢性疼痛会影响重建过程。

了解神经损伤的机制可能有助于治疗烧伤相关的神经疼痛。这一建议的分类是基于神经损伤的原因,旨在加强对烧伤相关神经疼痛的理解和管理。
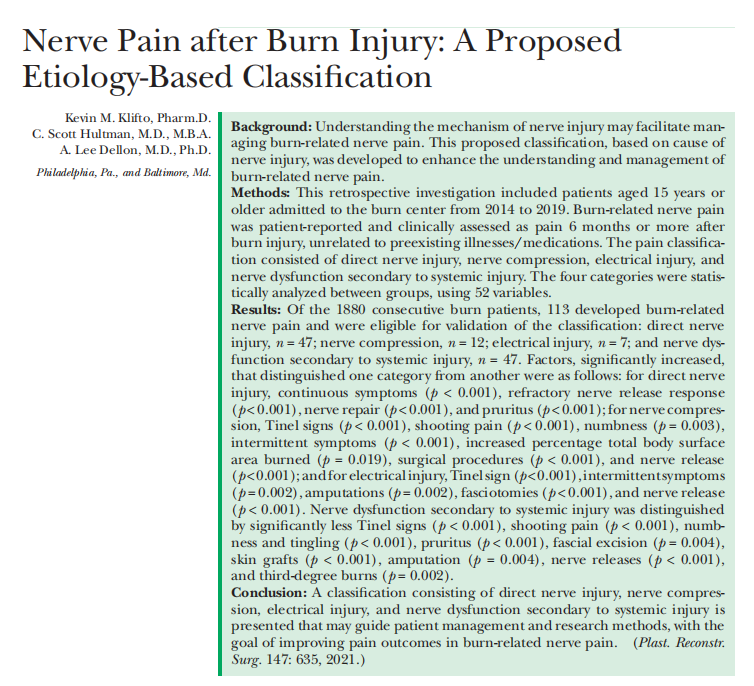
这项回顾性调查包括2014-2019年在烧伤中心就诊的15岁及以上患者。烧伤相关的神经疼痛是患者报告的,临床评估为烧伤后6个月或更长时间的疼痛,与先前存在的疾病/药物无关。
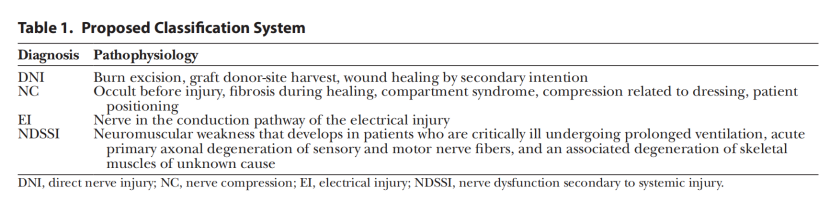
疼痛分类包括直接神经损伤、神经压迫、电损伤和继发于全身损伤的神经功能障碍。使用52个变量对这四个类别进行了组间统计分析。
在1880例连续烧伤患者中,113例出现烧伤相关的神经疼痛(患病率为6%),符合分类标准。
113例烧伤相关神经损伤患者中,47例为直接神经损伤,12例为神经压迫,7例为电损伤,47例为全身损伤继发神经功能障碍。
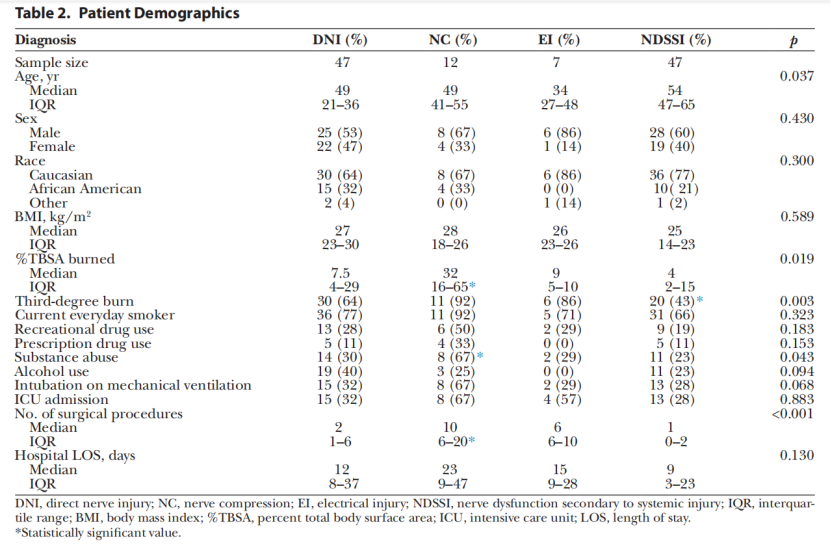
直接神经损伤与持续性疼痛症状(p<0.001)和瘙痒(p<0.001)显著相关(表3)。神经修复与慢性疼痛的缓解显著相关(p<0.001)(表4)。
神经压迫与烧伤总面积百分比增加(p=0.019)、烧伤前滥用物质(p=0.005)和更多的外科手术(p<0.001)显著相关(表2)。与神经压迫相关的疼痛特征是Tinel征阳性(p<0.001)、枪击痛(p<0.001)、麻木(p=0.003)和间歇性症状(p<0.001)(表3)。神经受压者筋膜切除显著增加(p=0.002)(表5)。羟色胺-去甲肾上腺素再摄取抑制剂(p<0.001)、阿片类药物(p<0.001)和神经松解治疗(p<0.001)在神经压迫相关疼痛中的使用显著较高(表4和表6)。压迫损伤与这些患者的总体并发症显著相关(p=0.003)(表7)。
与其他类别相比,电损伤与Tinel阳性体征(p<0.001)和间歇性症状(p=0.002)显著相关(表3)。电击伤患者截肢(p=0.002)和筋膜切开术(p<0.001)明显增多。在这一类别中,压迫,然后是神经松解,在治疗疼痛方面明显更高(p<0.001)(表4)。
全身损伤继发的神经功能障碍与较少的三度烧伤显着相关(p=0.002)(表2)。疼痛特征包括与其他类别相比,治疗后长期疼痛评分降低(p<0.001)、无体征和症状(tinel征)(p<0.001)、刺痛(p<0.001)、麻木(p<0.001)、刺痛(p<0.001)和瘙痒(p<0.001)。与筋膜切除(p=0.004)和皮肤移植(p<0.001)相比,外科烧伤治疗与全身损伤相关的明显较少。与其他类型的疼痛相比,全身损伤患者没有截肢(p=0.004)(表5)。与其他类型的疼痛[激光(p=0.002)和物理治疗/职业治疗(p<0.001)]相比,全身损伤所需的神经疼痛的手术和非手术治疗要少得多。与其他类型的疼痛相比,全身损伤患者没有神经释放(p<0.001)。



该研究提出了由直接神经损伤、神经压迫、电损伤和继发于全身损伤的神经功能障碍组成的分类方法,可指导患者的治疗和研究方法,以改善烧伤相关神经疼痛的疼痛结局。
原始文献:
Klifto Kevin M,Hultman C Scott,Dellon A Lee,Nerve Pain after Burn Injury: A Proposed Etiology-Based Classification.[J] .Plast Reconstr Surg, 2021, 147: 635-644.
DOI: 10.1097/PRS.0000000000007639
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#PRS#
40
优秀
74
学习到了很多
79
一积分
70
#镇痛#
52
谢谢梅斯提供这么好的信息,学到很多
62
关注提高患者生存质量
91