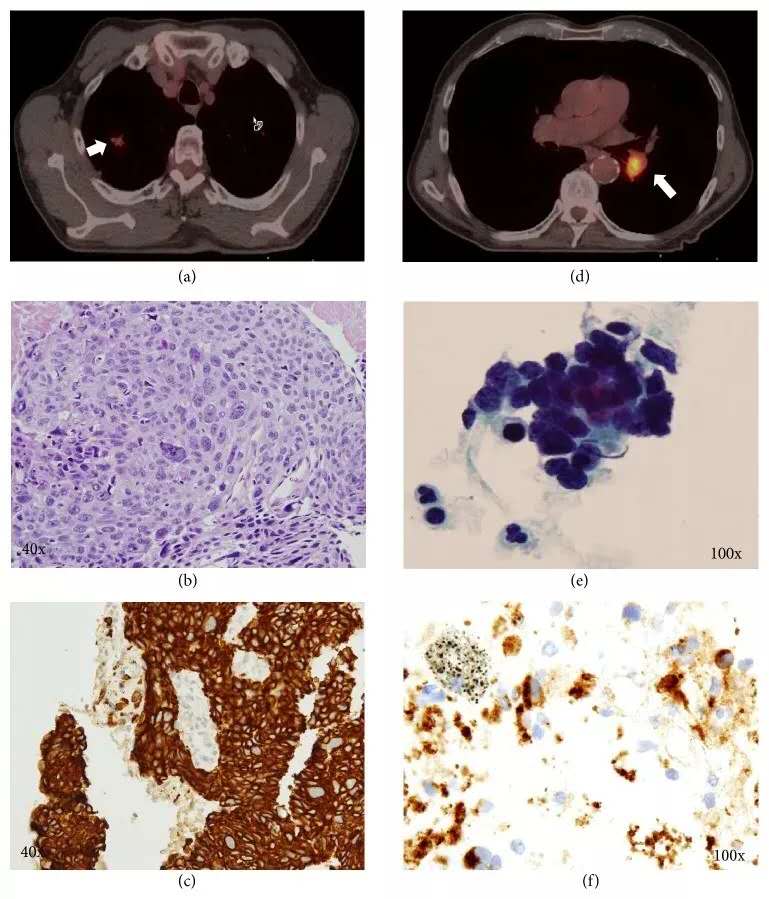
Thorax:肺癌后第二原发癌和更高级吸烟相关原发癌的发病率
2019-02-19 xiangting MedSci原创
从初次诊断开始,肺癌幸存者后续肺癌、喉癌、头颈癌和食管鳞状细胞癌发病率升高至少持续10年。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发病率#
38
学习学习努力学习
81
学习了谢谢分享
86
好文章,点赞啦!认真学习,谢谢分享给广大同好!
79