Cell rep:致病性 Th17 细胞调控新机制
2018-05-25 清华免疫 细胞
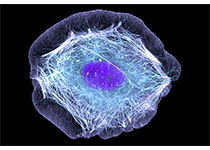
2018 年 5 月 22 日,清华大学免疫学研究所董晨课题组在《Cell Reports》在线发表题为 “Regulation of pathogenic T helper 17 cell differentiation by steroid receptor coactivator-3”的研究论文。该论文揭示了 SRC3 在致病性 Th17 细胞发育中的重要作用及其调控机制,为 Th17 细胞

SRC3调控致病性Th17细胞发育机制
Th17 细胞由董晨课题组等发现,与多种自身性免疫疾病密切相关,并在不同环境和疾病中发挥保护性或致病性等不同功能。其早期发育受多种细胞因子和转录因子的调控,RORγt 为关键的调控 Th17 细胞发育的谱系特异性转录因子。目前,尽管有一系列研究阐述 Th17 细胞发育调控机制,但 Th17 细胞的不同功能如何被调控、RORγt 具体如何发挥作用仍不十分清楚。
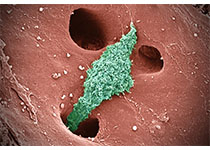
Steroid-receptor coactivator-3 (SRC3) 是一种核受体共激活蛋白,与核受体 RID 区域和组蛋白乙酰酶 p300 结合促进靶基因转录。在本研究中,董晨课题组发现 T 细胞中 SRC3 的条件性敲除,能特异性抑制 IL-1/IL-6/IL-23 诱导的致病性 Th17 细胞的发育,影响 IL17a、IL17f、IL23r、IL22 等 Th17 细胞特异性基因的表达,而不影响其他辅助性 T 细胞、调节性 T 细胞和非致病性 Th17 细胞的发育。同时,SRC3 缺失能降低 Th17 细胞致病性,显着降低 EAE 模型的发病率并缓解发病进程及严重程度。
利用高通量测序技术,进一步研究发现,Il1r1 是 SRC3 的重要调控靶点,在 SRC3 缺陷 T 细胞中过表达 Il1r1 能有效地重新促进 Th17 细胞的发育并恢复在 EAE 模型中的致病性功能。一方面,SRC3 能直接与 RORγt 结合,进一步被招募到 IL17a 和 IL1r1 等区域促进其转录;另一方面,SRC3 缺陷能通过影响组蛋白甲基化和乙酰化修饰影响转录活性,并减少组蛋白乙酰化酶的结合。
董晨教授为该研究的通讯作者,董晨实验室以前的博士后 Kentaro Tanaka 和学生 Gustavo J. Martinez 是该文的共同第一作者,其合作者来自美国西雅图系统生物学研究所,休士顿贝勒医学院以及清华大学等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
41
#致病性#
45
#CEL#
28
#Th17#
45
学习了谢谢分享
76
学习了受益匪浅
57