J Invest Dermatol:CD4+T细胞的增殖和补体系统的参与泛发性脓疱型银屑病MPO的缺陷
2022-01-14 医路坦克 MedSci原创
广泛性脓疱型银屑病(GPP)属于较为罕见的脓疱亚型。 未来评估受影响的细胞类型和途径的研究将显示它们在GPP发病机制中的作用,并表明研究结果是否可以转移到急性表皮情况。
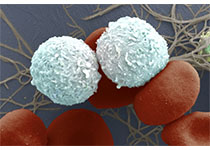
银屑病是一种常见的自身免疫性疾病,在发达国家约有2-3%的人口受其影响,而广泛性脓疱型银屑病(GPP)属于较为罕见的脓疱亚型。GPP是一种多系统疾病,通常发生在急性,潜在的威胁生命的事件,需要住院治疗。组织学上,中性粒细胞为主的无菌表皮脓疱是GPP的特征。编码白介素-36受体拮抗剂(IL-36Ra,基因IL36RN)的基因变异已被确定为致病基因。IL-36受体(IL-36R)及其配体前体IL-36α、-β和-γ主要在角质形成细胞中表达,而IL-36R在骨髓源性细胞中的表达已进行过描述:小鼠和人的树突状细胞以及人的中性粒细胞。
IL-36信号转导导致核因子-κB和丝裂原活化蛋白激酶的激活,导致促炎细胞因子的产生,如IL-8。在IL36RN变异的患者中,IL-36途径有利于角质形成细胞中促炎细胞因子的产生。针对IL-36R的治疗在有和没有IL36RN变异的患者中显示了良好的反应,突出了这一途径在GPP中的中心作用。
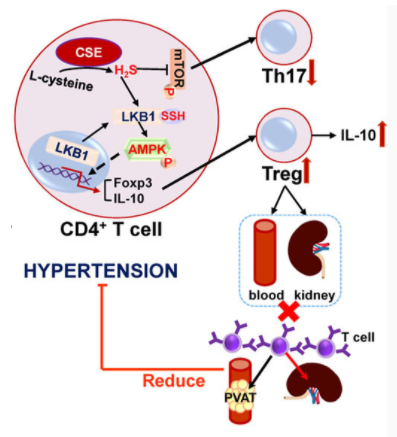
尽管IL36RN和MPO的变异可以影响免疫细胞,但目前还没有对中性粒细胞和外周血单个核细胞(PBMC)亚群以及它们的差异基因表达与MPO基因型的关系进行系统的分析。
我们使用PBMCs的单细胞RNA测序(ScRNAseq)和稳定期中性粒细胞的RNA测序来评估MPO缺陷患者的转录组。
细胞表面和细胞内标志物的流式细胞术分析验证了scRNAseq数据多模式参考图对细胞类型的标注:GPP中CD4+细胞毒性T淋巴细胞(CTL)和其他CD4+效应细胞比例增加,而单纯CD4+T细胞比例明显降低。标志CD4+CTL和CD8+效应记忆T细胞(TEMs)的FGFFBP2在具有致病变异的GPP患者中的表达高于非携带者(p=0.0015)。在中性粒细胞中,差异表达基因(Deg)明显富含经典补体激活途径的基因。
未来评估受影响的细胞类型和途径的研究将显示它们在GPP发病机制中的作用,并表明研究结果是否可以转移到急性表皮情况,以及CD4+CTL是否耗尽或失活可能是合理的治疗方法。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CD4#
38
#泛发性#
50
#EST#
33
#CD4+#
32
#CD4+T细胞#
39
#MPO#
41