Circ Res:醛固酮/盐皮质激素受体通路在二尖瓣脱垂发展中的新作用
2021-07-14 MedSci原创 MedSci原创
二尖瓣脱垂(MVP)是最常见的瓣膜疾病之一。然而,二尖瓣小叶组织中涉及纤维粘液瘤变化的分子和细胞机制尚未阐明。醛固酮 (Aldo) 促进心肌纤维化,而 MR(盐皮质激素受体)拮抗剂 (MRA) 通过减
二尖瓣脱垂(MVP)是最常见的瓣膜疾病之一。然而,二尖瓣小叶组织中涉及纤维粘液瘤变化的分子和细胞机制尚未阐明。醛固酮 (Aldo) 促进心肌纤维化,而 MR(盐皮质激素受体)拮抗剂 (MRA) 通过减少心脏纤维化来改善心脏功能。近日,研究人员探究了Aldo/MR 在与 MVP 相关的纤维粘液瘤修饰中的作用,研究结果已发表于Circ Res。

Aldo增强瓣膜间质细胞活化标志物并诱导瓣膜内皮细胞的内皮-间充质转化,导致蛋白多糖分泌增加。MRA 阻止了上述所有影响。细胞因子阵列显示 CT-1(心肌营养素-1)是 Aldo 诱导的瓣膜间质细胞活化和蛋白多糖分泌的介质,CD(分化簇)14 是 Aldo 诱导的内皮-间充质转化和蛋白多糖分泌的介质瓣膜内皮细胞。在通过去甲右芬氟拉明给药产生的 MVP 实验小鼠模型中,MRA 治疗降低了二尖瓣厚度和蛋白多糖含量。内皮特异性 MR 缺失阻止了由去甲右芬氟拉明给药引起的纤维粘液瘤变化。此外,在接受 MRA 治疗的 MVP 患者的二尖瓣中,蛋白多糖表达略低。
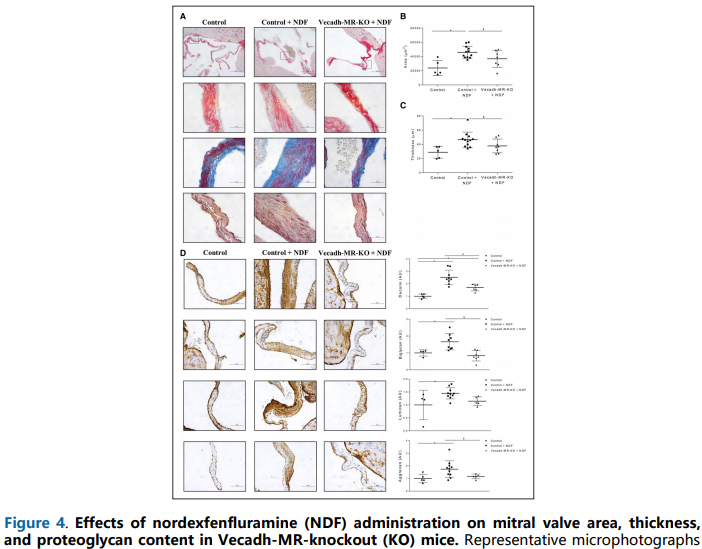
综上,这些发现首次证明,Aldo/MR通路调节与MVP发展相关的瓣膜间质细胞和瓣膜内皮细胞的表型、分子和组织学变化。MRA 治疗似乎是减少 MVP 纤维粘液瘤改变的有希望的选择。
原始出处:
Jaime Ibarrola, et al., A New Role for the Aldosterone/Mineralocorticoid Receptor Pathway in the Development of Mitral Valve Prolapse. Circ Res. 2020 Jul 17;127(3):e80-e93. doi: 10.1161/CIRCRESAHA.119.316427.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新作用#
35
#二尖瓣脱垂#
33
#醛固酮#
36
#二尖瓣#
33
#皮质激素#
35