NEJM:ADC药物效果惊艳,延长晚期乳腺癌患者无进展生存期50%
2022-06-08 王聪 “生物世界”公众号
乳腺癌可以分为 HER2 阳性乳腺癌(约占20%)和 HER2 阴性乳腺癌(约占80%),而这些 HER2 阴性乳腺癌患者中,大约有一半实际上表达低水平的 HER2。而目前可用的 HER2 靶向疗法对
乳腺癌,是女性中最常见的癌症,而在2020年,乳腺癌取代肺癌,已成为全球第一大癌症,WHO国际癌症研究署(IARC)发布的2020年全球最新癌症负担数据显示,2020年全球乳腺癌新发病例高达226万例,死亡68万例。在我国,乳腺癌的发病率也在逐年提升,据WHO预测,2020年中国新增乳腺癌病例高达41万。
乳腺癌可以分为 HER2 阳性乳腺癌(约占20%)和 HER2 阴性乳腺癌(约占80%),而这些 HER2 阴性乳腺癌患者中,大约有一半实际上表达低水平的 HER2。而目前可用的 HER2 靶向疗法对这些低表达 HER2(HER2-low)乳腺癌患者无效。
2022年6月5日,《新英格兰医学杂志》(NEJM)发表了由纪念斯隆凯特琳癌症中心(MSKCC)的 Shanu Modi 博士领导的一项 ADC 药物 Enhertu 治疗 HER2 低表达(HER2-Low)晚期乳腺癌患者的3期临床试验。论文题为:Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer。
这项3期临床试验显示,与接受标准化疗的患者相比,Enhertu 将 HER2 低表达晚期乳腺癌患者的无进展生存期延长了约50%,将总生存期延长了月40%。
这也是首次证明可以通过药物靶向低表达的 HER2 蛋白并发挥癌症治疗效果。大约一半的之前被认为是 HER2 阴性的乳腺癌患者实际上是 HER2 低表达(HER2-low)乳腺癌,这意味着她们可以受益于该 ADC 药物。这为成千上万的晚期乳腺癌患者开辟了新的治疗可能性。
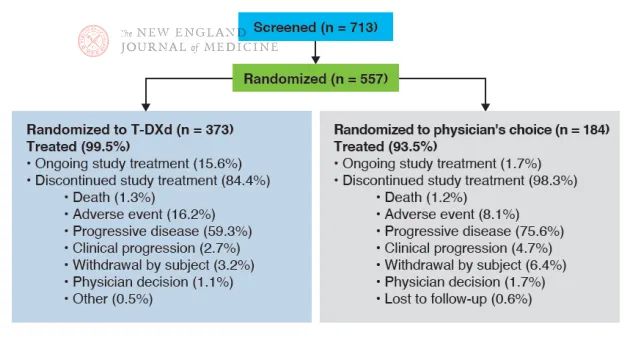
这项3期临床试验共有557名患者参与,是之前已经接受过一线或二线化疗的 HER2 低表达的转移性晚期乳腺癌患者。HER2 低表达的定义是免疫组化(IHC)分析得分为1+,或 IHC 得分为2+,但原位杂交结果为阴性。
Enhertu(Trastuzumab Deruxtecan),是一款由阿斯利康和第一三共合作开发的抗体偶联药物(ADC),于2019年获得 FDA 批准用于治疗不可切除或转移性 HER2 阳性乳腺癌患者。这款 ADC 药物,是将 HER2 单抗 Trastuzumab(曲妥珠单抗) 与拓扑异构酶1抑制剂 exatecan 衍生物(DXd)连接起来,从而在阻断 HER2 蛋白的同时,发挥化学毒素的抗癌作用。

Enhertu 的费用约为14000美元/月
患者按照2:1的比例随机分配接受 ADC 药物 Enhertu(Trastuzumab Deruxtecan)治疗或接受标准化疗。这557名 HER2 低表达的转移性晚期乳腺癌患者中,494名(88.7%)为激素受体阳性(HR+),63名(11.3%)为激素受体阴性(HR-)。
在激素受体阳性(HR+)队列中,ADC 药物 Enhertu 治疗组的中位无进展生存期为10.1个月,标准化疗组为5.4个月,总生存期为分别为23.9个月和17.5个月。
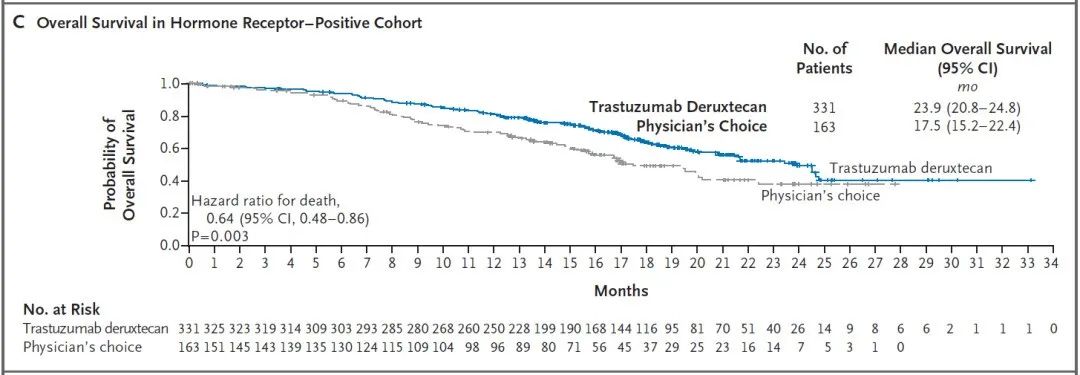
在所有患者中,ADC 药物 Enhertu 治疗组和标准化疗组的中位无进展生存期分别为9.9个月和5.1个月,总生存期分别为23.4个月和16.8个月。

ADC 药物 Enhertu 治疗组的患者中有52.6%发生了3级或更高级别的不良事件,而这一数据在标准化疗组中是67.4%。此外,ADC 药物 Enhertu 治疗组的患者中有12.1%发生了与药物治疗相关的间质性肺病或肺炎,其中有3人(0.8%)因此死亡。
总的来说,这项涉及HER2 低表达(HER2-low)的转移性/晚期乳腺癌患者的3期试验显示,与标准化疗相比,ADC 药物 Enhertu 治疗显着延长了患者的无进展生存期和总生存期。
原始出处:
Shanu Modi, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. NEJM, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#生存期#
50
#无进展生存期#
38
#乳腺癌患者#
57
NEJM上果然牛,感谢梅斯更新及时
44