Clin Cancer Res:伊匹单抗+纳武单抗治疗脑转移的黑色素瘤的3期试验的长期随访结果
2021-09-02 Nebula MedSci原创
与福替莫司汀相比,伊匹单抗联合纳武单抗可显著提高无症状脑转移的黑色素瘤患者的总存活率和长期存活率
2 期试验显示,伊匹单抗联合福替莫司汀(Fotemustine)和伊匹单抗联合纳武单抗治疗黑色素瘤脑转移的活性令人鼓舞。NIBIT-M2 试验是首个对比这些方案与福替莫司汀联合用于已发生脑转移的黑色素瘤患者的 3 期试验。
本文报告了 NIBIT-M2 试验随访 4 年后的主要分析结果。
该试验招募了年满 18 岁的 BRAF 野生型或突变型的黑色素瘤患者,且要求受试患者有无症状的脑转移,但未针对脑转移进行过治疗。受试患者被随机(1:1:1)分至三组,分别接受福替莫司汀、伊匹单抗+福替莫司汀或伊匹单抗+纳武单抗治疗。主要终点是总生存期(OS)。
三组患者的总生存期
从2013年1月至2018年9月期间,分别有 27 位、26 位和 27 位接受了福替莫司汀、伊匹单抗+福替莫司汀或伊匹单抗+纳武单抗治疗。福替莫司汀组、伊匹单抗+福替莫司汀组和伊匹单抗+纳武单抗组的中位 OS 分别是 8.5 个月(95%CI 4.8-12.2)、8.2 个月(2.2-14.3)和 29.2 个月(0-65.1);伊匹单抗+福替莫司汀组与福替莫司汀组相比的 OS 的风险比(HR)为 1.09(95% CI 0.59–1.99; P=0.78);伊匹单抗+纳武单抗组与福替莫司汀组相比的 OS 的 HR 为 0.44(95% CI 0.22–0.87; P=0.017)。
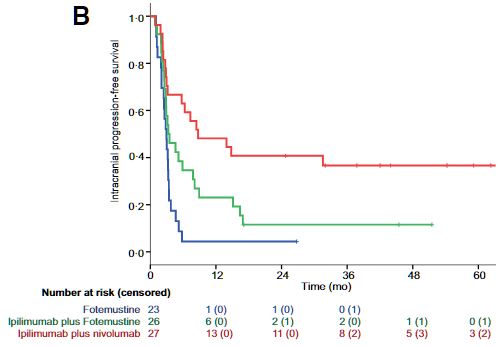
三组患者的无颅内进展生存期
伊匹单抗+纳武单抗组的 4 年存活率明显高于福替莫司汀组(41.0% vs 10.9%;P=0.015),而伊匹单抗+福替莫司汀组的 4 年存活率还低于福替莫司汀组(10.3%)。
不良事件发生率
福替莫司汀组、伊匹单抗+福替莫司汀组和伊匹单抗+纳武单抗组的3-4级治疗相关的不良事件的发生率分别为48%(11例)、69%(18例)和30%(8例),无治疗相关死亡。
总之,与福替莫司汀相比,伊匹单抗联合纳武单抗可显著提高无症状脑转移的黑色素瘤患者的总存活率和长期存活率。
原始出处:
Anna Maria Di Giacomo, et al. Primary Analysis and 4-Year Follow-Up of the Phase III NIBIT-M2 Trial in Melanoma Patients With Brain Metastases. Clin Cancer Res. DOI: 10.1158/1078-0432.CCR-21-1046 Published September 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#随访结果#
44
#色素#
43
#长期随访#
45
#3期试验#
48
#黑色素#
40
#黑色素#
33
学习了
69
学习
59