Eur J Heart Fail:射血分数保留的心衰患者运动时的心率和搏出量变化
2021-03-11 Nebula MedSci原创
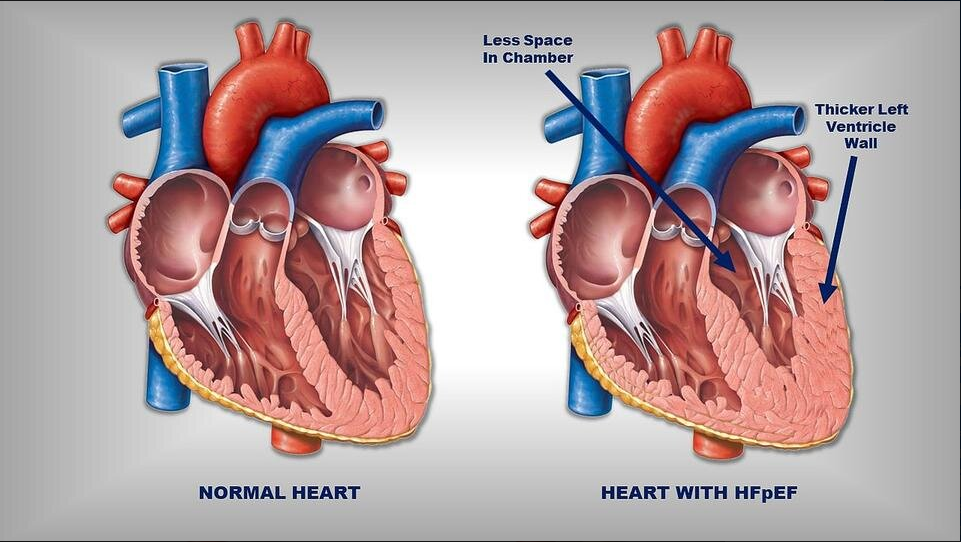
射血分数保留的心力衰竭(HFpEF)的一个标志是不同程度的运动能力受损
射血分数保留的心力衰竭(HFpEF)的一个标志是不同程度的运动能力受损。运动能力的主要决定因素是心输出量(CO),HFpEF患者的运动能力受损主要是在体力运动时不能根据外周需求增加CO。但是,目前HFpEF患者的CO构成(心率×每搏输出量)与运动量之间的关系鲜有报道。
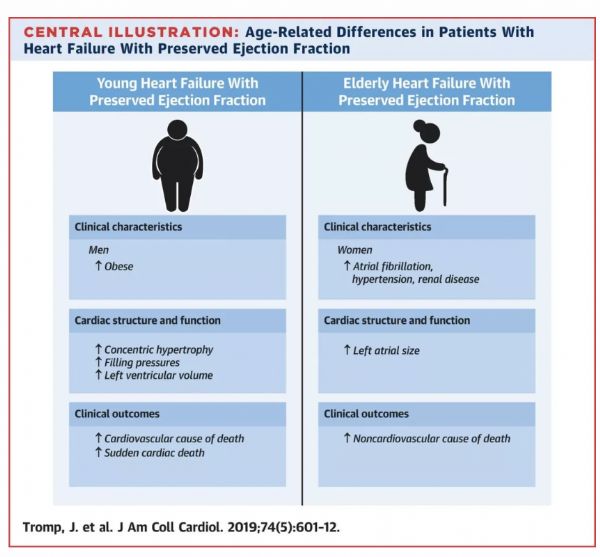
本研究旨在探究HFpEF患者对运动的心率和每搏量反应是否存在异质性,并描述与这些反应差异相关的可能临床表型。
采用了两个HFpEF的前瞻性试验(n=108)和一项健康受试者(n=42)在运动过程中有创血流动力学测量的数据。用回归模型分析中心血流动力学反应的差异。
心率和搏出量变化的相关性
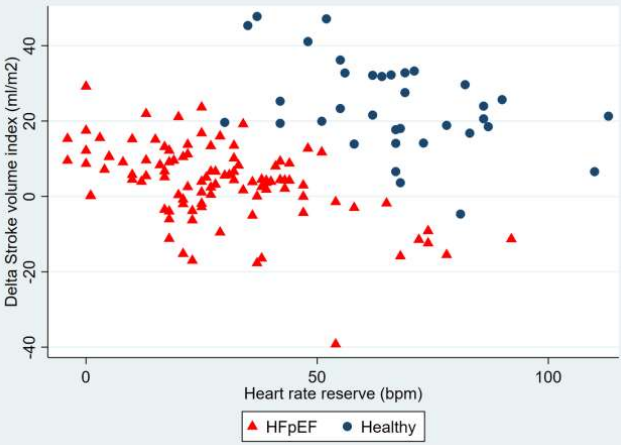
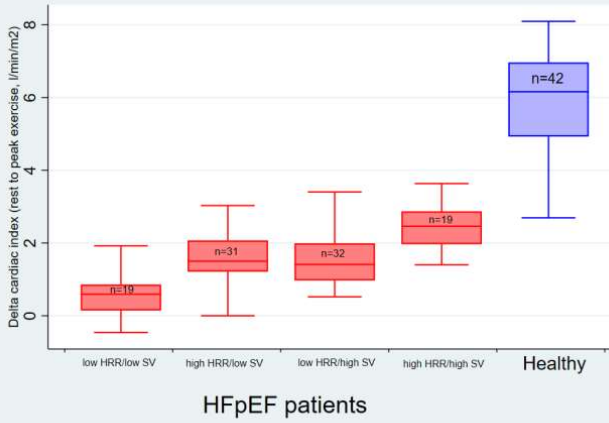
分析结果显示,39-56%的HFpEF患者和3-56%的健康受试者存在变时性功能不全,但部分HFpEF患者(n=47,44%)的心率增加与健康对照组相似。HFpEF患者的每搏输出量指数(SVI)增加较少(HFpEF:+4±10ml/m2,健康受试者:+24±12ml/m,p<0.0001),实际上,28%的患者在运动高峰时的SVI下降。
心指数的变化
在HFpEF患者中,安静时较高的BMI和较低的SVI与运动时较少的心率增加有关,而较高的静息心率和ACE抑制剂/血管紧张素受体阻滞剂(ARB)的使用与较多的SVI增加有关。
总之,HFpEF患者运动时的血流动力学反应具有很明显的异质性,高达56%的患者存在变时性功能不全,28%的患者的SVI增加受损。这表明血流动力学运动试验可能有助于确定哪些HFpEF患者可能受益于针对每搏输出量和变时性反应的干预。
注释:
心脏变时性功能:正常窦房结在神经、体液等因素调节下,根据机体不同状况,在较大范围内改变心率的快慢以满足机体供血、代谢的需要,这种功能称为心脏变时性功能。
心脏变时性功能不全:窦房结对运动或代谢等病理生理变化丧失了应用的正常心率反应,即心率增快未达到一定程度,称为心脏变时性功能不全。
原始出处:
Wolsk Emil,Kaye David M,Komtebedde Jan et al. Determinants and consequences of heart rate and stroke volume response to exercise in patients with heart failure and preserved ejection fraction. Eur J Heart Fail, 2021, 10.1002/ejhf.2146
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#射血分数保留#
29
棒
49
学习了
0
#ART#
33
#心衰患者#
39
#HEART#
32