J Clin Periodontol:镰状细胞贫血患者的铁过载及牙周状况
2020-05-31 网络 网络
本文旨在研究镰状细胞贫血(SCA)患者的铁过载、牙周状况和牙周炎程度的相关性。
本文旨在研究镰状细胞贫血(SCA)患者的铁过载、牙周状况和牙周炎程度的相关性。
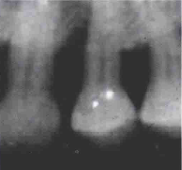
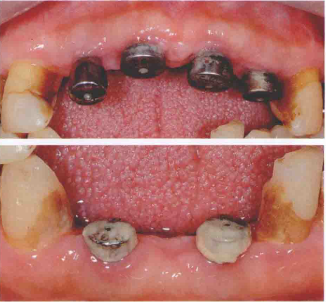
本研究共纳入123名患者,对患者每颗牙齿六个位点的临床附着水平(CAL)和探诊深度(PD)进行评估,并使用影像学技术评估牙槽骨吸收水平。研究结果包括牙周状况(CAL≥3mm,CAL≥5mm;PD≥4mm,PD≥6mm)和牙周炎程度(按牙槽骨骨吸收与年龄的比例确定)。从病历中获取血清转铁蛋白饱和度和铁蛋白水平。调整后的模型中包含的协变量(合并症、肤色、社会经济水平和血管闭塞危机)由DAGs定义。
结果发现,血清转铁蛋白饱和水平与CAL≥3mm、CAL≥5mm、PD≥4mm、PD≥6mm、PD≥6mm等位点数具有明显的阳性相关关系。血清转铁蛋白饱和度>45%的患者出现快速进展性牙周炎的可能性高出1.93倍。
因此,高血清转铁蛋白饱和水平与SCA的牙周炎的范围和程度有关。
原文出处:
Susilena Arouche Costa, Iron over load and periodontal status in patients with sickle cell anaemia: A cases eries, journal of clinical periodontology, 2020 June, doi:10.1111/jcpe.13284
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#铁过载#
32
#PE#
32
#牙周状况#
35
#牙周#
31
#镰状细胞贫血#
33
#镰状细胞#
42