Gastroenterology:HCV感染引起的与肝癌风险相关的表观遗传改变在持续的病毒学应答后持续存在
2019-03-28 佚名 临床肝胆病杂志
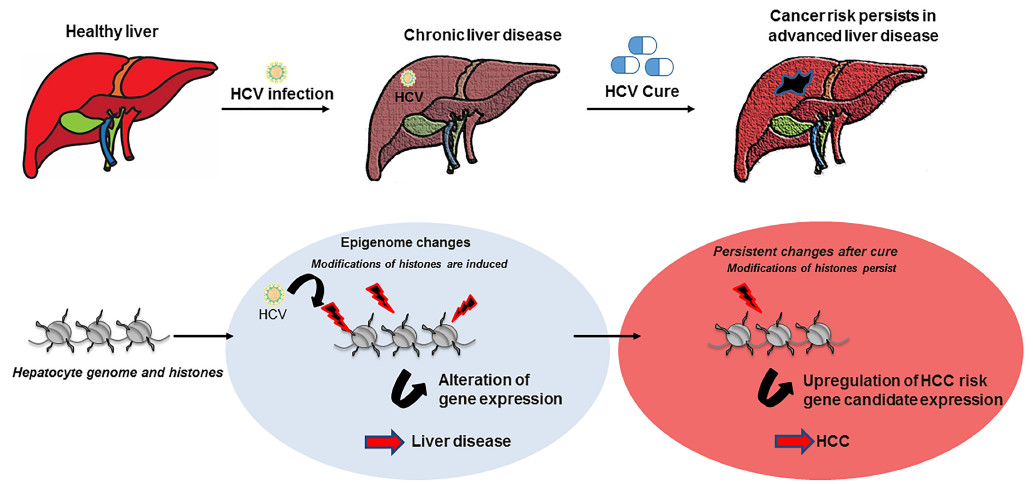
慢性HCV感染是肝癌的重要危险因素。服用直接抗病毒药物(DAA)获得持续的病毒学应答,可以减少但不能消除丙型肝炎发展为肝癌的风险,在晚期肝硬化患者中这种风险更高。在患者和人源化肝脏小鼠中,研究者观察了HCV引起的表观遗传学改变,这种改变可能会影响丙型肝炎患者在直接抗病毒治疗后罹患肝癌的风险。
慢性HCV感染是肝癌的重要危险因素。服用直接抗病毒药物(DAA)获得持续的病毒学应答,可以减少但不能消除丙型肝炎发展为肝癌的风险,在晚期肝硬化患者中这种风险更高。在患者和人源化肝脏小鼠中,研究者观察了HCV引起的表观遗传学改变,这种改变可能会影响丙型肝炎患者在直接抗病毒治疗后罹患肝癌的风险。
在欧洲和日本收集6例无HCV感染(对照)、18例慢性HCV感染、8例DAA治愈的慢性HCV感染、13例干扰素治愈的慢性HCV感染、4例慢性HBV感染和7例非酒精性脂肪性肝炎患者,对这些患者的肝组织进行了全基因组序列分析。对HCV引起的表观遗传改变和其他肝病病因相关的改变进行比较分析。UPA/SCID小鼠移植人肝细胞,建立人源化肝脏小鼠,注射HCV感染患者血清样品,给予DAA根除病毒。与肝癌风险相关的通路通过整合通路分析被确定,并在8例服用DAA获得持续病毒学应答患者的肝癌组织的配对分析中得到了验证。
研究者发现,慢性HCV感染可引起H3K27ac的基因组特异性改变,这组基因与mRNAs和蛋白质的表达变化有关。在DAA或干扰素治疗获得持续病毒学应答后,这种基因改变是持续存在的。对人源化肝脏小鼠和患者的肝组织的整合通路分析表明,HCV引起的表观遗传改变与肝癌风险有关。计算分析表明,鞘氨醇激酶(SPHK)1的表达增加与肝癌风险有关。在一组独立的HCV相关肝硬化患者(n=216)中验证了这些发现,其中21例患者达到了病毒学清除。
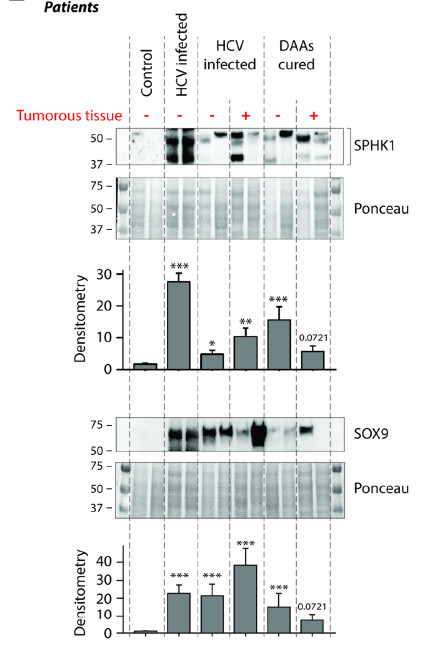
通过对DAA治疗持续病毒学应答和无持续病毒学应答患者的肝组织进行分析发现了与肝癌风险相关的表观遗传和基因表达的改变,这些改变可能是预防丙型肝炎患者抗病毒治疗后罹患肝癌的靶点。
原始出处:Hamdane N1, Jühling F1, Crouchet E1, et al. HCV-induced Epigenetic Changes Associated With Liver Cancer Risk Persist After Sustained Virologic Response. Gastroenterology. 2019 Mar 2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
38
#AST#
38
#癌风险#
41
#Gastroenterol#
46
#病毒学应答#
39
#HCV#
39
#Gastroenterology#
25
#病毒学#
32
#HCV感染#
0
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
64