默克27.5亿美元收购VelosBio,获得靶向ROR1的抗体-药物偶联物(ADC)
2020-11-09 MedSci原创 MedSci原创
1期临床试验结果表明:VLS-101分别让47%的套细胞淋巴瘤患者和80%的弥漫性大B细胞淋巴瘤患者产生应答。
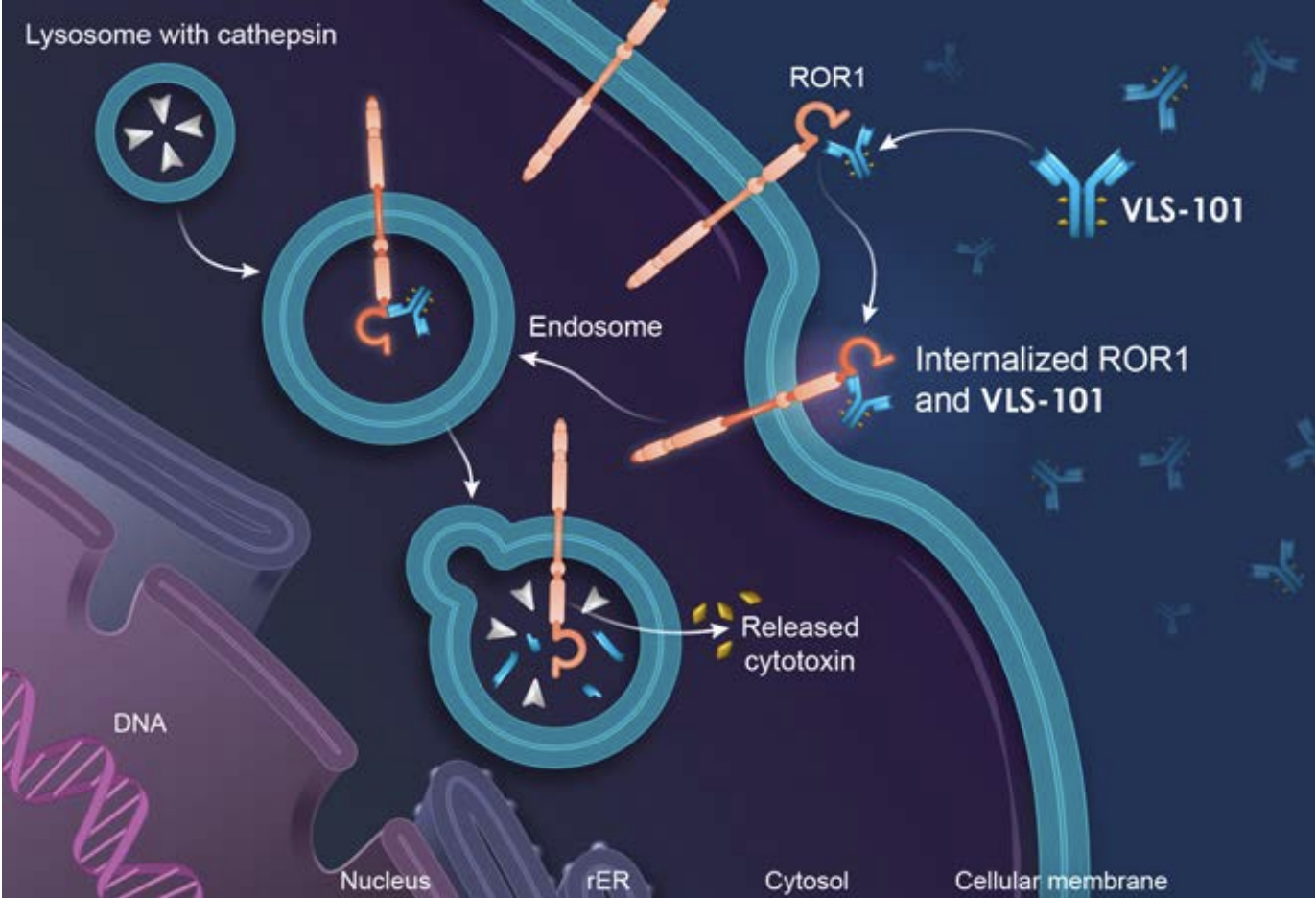
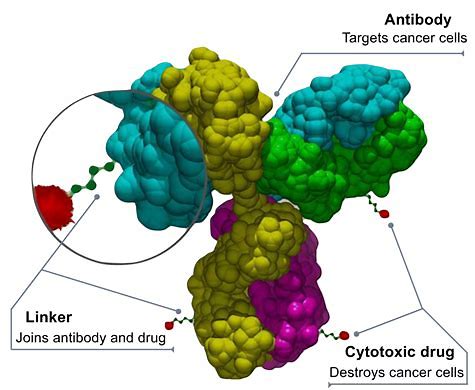
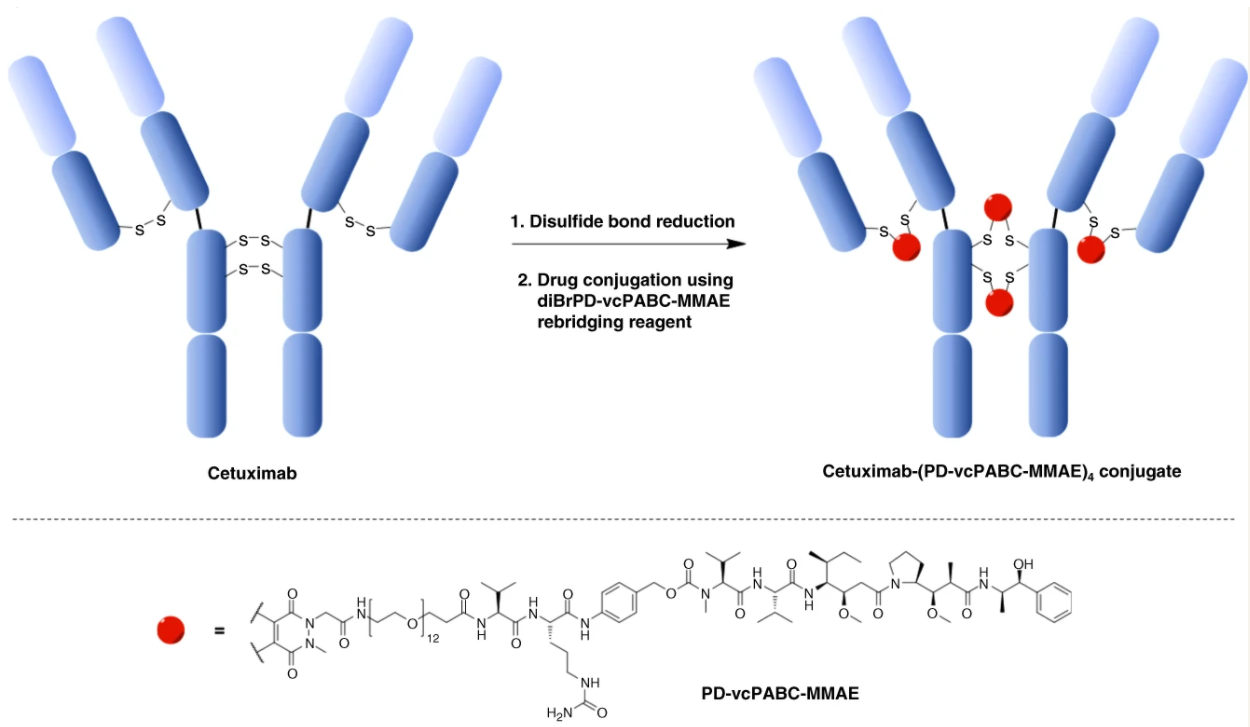
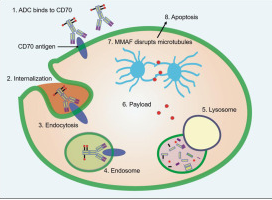
默克公司(MSD)同意以27.5亿美元收购VelosBio以获得多种癌症疗法。VelosBio正在开发针对酪氨酸激酶样孤儿受体1(ROR1)的抗体-药物偶联物(ADC)VLS-101,据研究发现ROR1在多种癌症中均过表达。
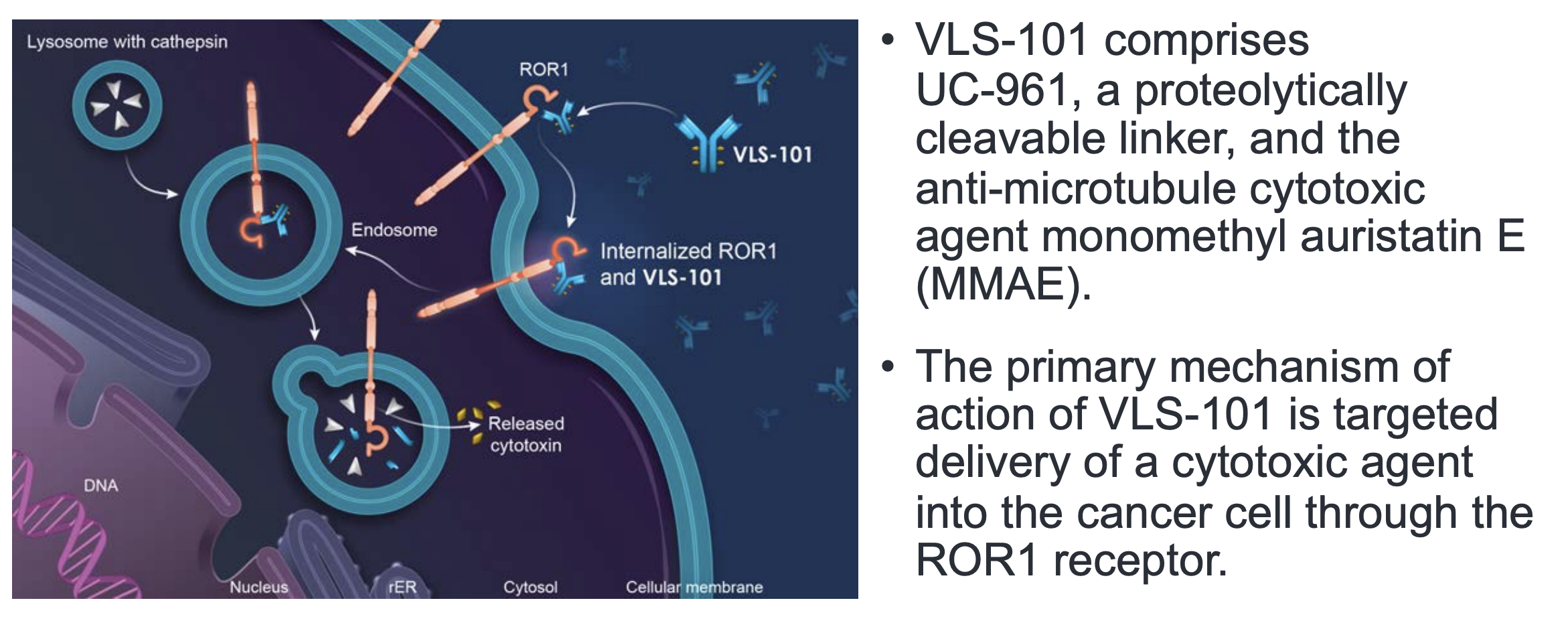
图片来源:VelosBio官网
VLS-101目前正在1期和2期试验中研究用于治疗血液系统恶性肿瘤和实体瘤患者。根据默克公司的说法,VLS-101在早期临床试验中显示了可控的安全性和抗肿瘤活性。
该ADC药物的1期临床试验结果表明VLS-101的治疗,分别让47%的套细胞淋巴瘤(MCL)患者和80%的弥漫性大B细胞淋巴瘤(DLBCL)患者产生应答。
10月,VelosBio宣布启动一项2期临床试验,以研究VLS-101用于治疗实体瘤患者,包括三阴性乳腺癌(TNBC),包括HER2受体阳性和阴性的乳腺癌和非鳞状非小细胞肺癌(NSCLC)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗体-药物偶联物#
32
#Bio#
23
厉害了
70
#默克#
36
学习了谢谢
86
学习了,谢谢分享
80