乳腺癌是全球女性发病率最高的恶性肿瘤。全球范围内,乳腺癌无论是从发病率还是致死率上,都给人类健康带来了极大的威胁。2020年底,世界卫生组织国际癌症研究机构(IARC)最新发布数据:乳腺癌已取代肺癌成为全世界最常见的癌症。
他莫昔芬是一种非甾体类选择性雌激素受体调节剂(SERM),主要用作绝经前女性和部分绝经后女性雌激素受体阳性乳腺癌的辅助治疗。在全球范围内,他莫昔芬从上世纪70年代开始被用于临床治疗,至今已有近半个世纪的历史。
该药也用于乳腺癌风险较高女性的化学预防,但同时有增加子宫病变的风险,包括子宫内膜息肉、子宫内膜癌与子宫内膜增生、子宫肉瘤及子宫癌肉瘤的风险。因此,如何对他莫昔芬调整用量使得更好减轻副作用同时不影响药效是一个迫在眉睫的问题。
乳房造影密度变化是他莫昔芬治疗反应的代表。最近,来自世界著名研究所瑞典卡洛琳卡医学院的专家测试了较低剂量的他莫昔芬是否能达到在降低乳腺造影密度的同时减轻副作用。相关结果发表在ASCO期刊《临床肿瘤学杂志》(JCO)。
该研究为瑞典乳腺钼靶X线筛查计划的一部分(KARISMA II期试验)。纳入40-74岁的妇女进行为期6个月的双盲、六臂、随机安慰剂对照、非劣效剂量测定。所有1439名参与者按绝经状态分层,其中1230名参与者进行意向治疗分析。
该研究以接受20mg治疗作为标准剂量。主要的研究结局是接受安慰剂、1、2.5、5和10mg治疗的参与者乳腺密度下降至少与20mg组的中位数下降幅度相同。非劣势幅度为17%。次要结果是临床症状的减少。
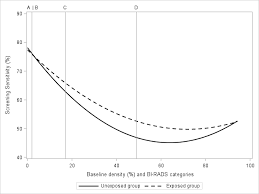
结果显示,在2016年10月1日至2019年9月30日期间招募了1439名参与者,分别为566名和873名绝经前和绝经后妇女。绝经前女性在服用2.5、5和10mg他莫昔芬后,乳腺造影密度减少与20mg标准计量类似,后者中位降低幅度为10.1%,但绝境后女性没有观察到上述现象。
与20mg标准剂量组相比,2.5、5和10mg组的严重血管述所症状(潮热、冷汗和盗汗)发生率减少了约50%。为此,该试验主要研究员,卡罗林卡研究所Per Hall教授指出:“减少用药剂量可能在减少副作用的同时让更多患者完成治疗。”
综上,绝经前妇女在服用2.5mg他莫昔芬时,乳腺密度降低幅度与标准剂量20mg相当,但副作用更少。未来的研究应该测试2.5mg的他莫昔芬是否能降低原发性乳腺癌的风险。
参考文献:
Mikael Eriksson, et al. Low-Dose Tamoxifen for Mammographic Density Reduction: A Randomized Controlled Trial. https://doi.org/10.1200/JCO.20.02598
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JCO#
39
#他莫昔芬#
57
#低剂量#
37
好消息
91
谢谢梅斯提供这么好的信息,学到很多
37
他莫替芬治疗乳腺癌
66
可以,很不错
72
学习了
75
学习学习
68