三重再摄取抑制剂(TRI)TNX-1600治疗创伤后应激障碍
2019-08-21 Allan MedSci原创
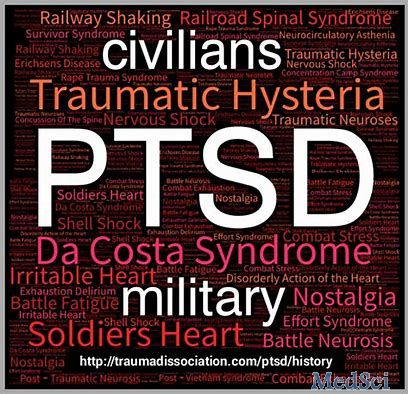
Tonix是一家临床阶段的生物制药公司,Tonix近日宣布,将扩大三重再摄取抑制剂(TRI)TNX-1600的适应症范围,以治疗创伤后应激障碍(PTSD)和潜在的其他中枢神经系统(CNS)疾病。
Tonix是一家临床阶段的生物制药公司,Tonix近日宣布,将扩大三重再摄取抑制剂(TRI)TNX-1600的适应症范围,以治疗创伤后应激障碍(PTSD)和潜在的其他中枢神经系统(CNS)疾病。
Tonix公司总裁兼首席执行官Seth Lederman博士说:“我们很高兴扩大我们的管道,并期待开发TNX-1600作为创伤后应激障碍的潜在治疗方法。我们计划利用在创伤后应激障碍中的临床经验来评估TNX-1600的治疗效果。创伤后应激障碍是一种异质性疾病,因此我们认为不同的创伤后应激障碍患者可能对不同的药物有反应。TNX-1600是我们开发创伤后应激障碍的第三个候选药物”。
原始出处:
http://www.firstwordpharma.com/node/1660599#axzz5xBxiqv3r
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#抑制剂#
21
#创伤#
28
#应激#
22