Lancet Respir Med: FeNO作为生物标志物指导儿童哮喘治疗策略是否有效?
2022-02-23 小文子 MedSci原创
RAACENO研究发现,症状指导哮喘治疗中增加FeNO并没有减少儿童哮喘急性加重。哮喘症状仍然是指导治疗的唯一工具。
呼出气一氧化氮(FeNO)指导哮喘治疗的益处尚不确定。Lancet Respir Med杂志发表的一项研究评价了哮喘儿童症状指导治疗的基础上加用FeNO指导哮喘治疗的效果。
RAACENO是一项多中心,随机对照3期试验,在英国的35家二级医疗机构和17家初级医疗机构进行。研究纳入确诊哮喘的患者,年龄6-15岁,处方吸入糖皮质激素,并在纳入研究前12个月内接受一个疗程口服糖皮质激素治疗至少一次哮喘急性加重。
将患者随机分配到FeNO加症状指导治疗组(干预组)和单独症状指导治疗组(标准治疗组)。未对患者以及临床和研究团队设盲。根据哮喘控制测试(ACT)或儿童ACT(CACT)评分、当前哮喘治疗、过去3个月对治疗的依从性和FeNO(干预组),基于网络算法给出个性化治疗建议。每隔3个月随访一次,持续12个月。主要结局是随机分组后12个月内接受口服糖皮质激素治疗的任何哮喘急性加重。
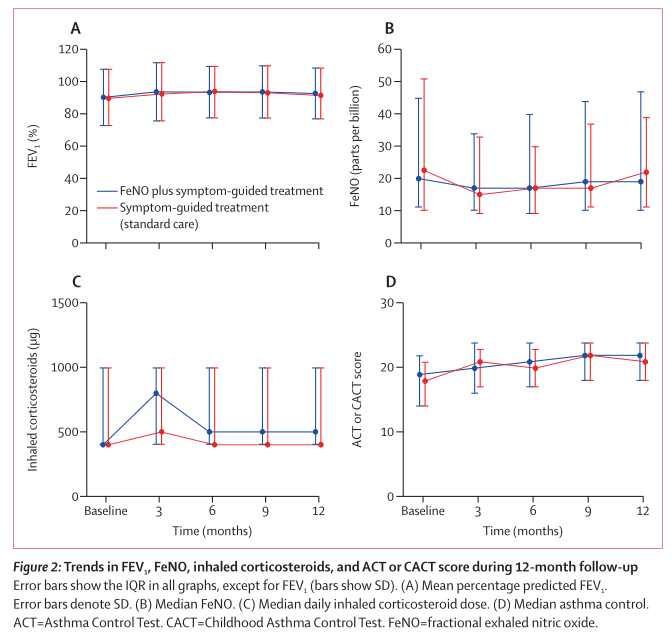
结果显示,2017年6月22日至2019年8月8日期间,纳入509名儿童,基线时,平均年龄为10.1岁(SD 2.6),308名(60.5%)为男性。中位FeNO为21 ppb(IQR 10-48),平均FEV1为89.6%(SD 18.0),每日吸入糖皮质激素的中位剂量为400 μg布地奈德当量(IQR 400-1000)。509例患者中有256例(50.3%)哮喘控制部分或完全控制。
509名患者中的506名(99%)患者出现了主要结局,干预组255名患者中有123名(48.2%)出现了主要结局,标准治疗组251名患者中有129名(51.4%)出现了主要结局,意向治疗校正OR为0.88(95%CI, 0.61~1.27; p = 0·49)。与标准治疗组相比,干预组发生主要结局的比例校正差异为-3.1%(-11.9%~5.6%)。
与标准治疗组相比,干预组出现首次急性加重时间的校正HR=0.92(95%CI, 0.71~ 1.18)。12个月随访期间,标准治疗组的中位ACT或CACT评分从18升高至21,中位PAQLQ评分从5.6升高至6.2。方案数据分析显示,165名干预组中的84人(50.9%)和153名标准护理组中的79人(51.6%)至少发生一次急性加重(校正OR=0.98,95%CI, 0.61~1.55; p=0.92)。
综上所述,RAACENO研究发现,症状指导哮喘治疗中增加FeNO并没有减少儿童哮喘急性加重。哮喘症状仍然是指导治疗的唯一工具。
原文出处:
Steve Turner, Seonaidh Cotton, et al, Reducing asthma attacks in children using exhaled nitric oxide (RAACENO) as a biomarker to inform treatment strategy: a multicentre, parallel, randomised, controlled, phase 3 trial, Lancet Respir Med 2022, DOI:https://doi.org/10.1016/S2213-2600(21)00486-0.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Lancet#
32
#标志物#
36
#儿童哮喘#
33
#生物标志#
32
#生物标志#
33
#Med#
40