J Clin Oncol:信迪利单抗联合安罗替尼治疗PD-L1阳性晚期宫颈癌
2022-02-24 Nebula MedSci原创 发表于威斯康星
信迪利单抗联合安罗替尼作为既往化疗失败的晚期宫颈癌患者的二线或晚线疗法是有效且安全的
既往研究已证实了派姆单抗在经化疗后进展的复发性或转移性晚期宫颈癌中的疗效和安全性。但是,目前尚无研究免疫疗法联合抗血管生成疗法用于程序性死亡配体 1(PD-L1)阳性的晚期宫颈癌(CA)患者的研究。
本研究旨在评估信迪利单抗联合安罗替尼作为 PD-L1 阳性的复发或转移性 (R/M) 宫颈癌的二线或后续治疗的疗效和安全性。
招募了不能耐受化疗或既往进行过系统化疗后进展的PD-L1阳性(综合阳性评分≥1)的转移性或复发性宫颈癌患者。第1天予以 200 mg 信迪利单抗,第1-14天每天予以 10 mg 安罗替尼,3周为一疗程。主要终点是客观缓解率(ORR)。次要终点包括无进展生存期(PFS)、总生存期(OS)和疾病控制率。
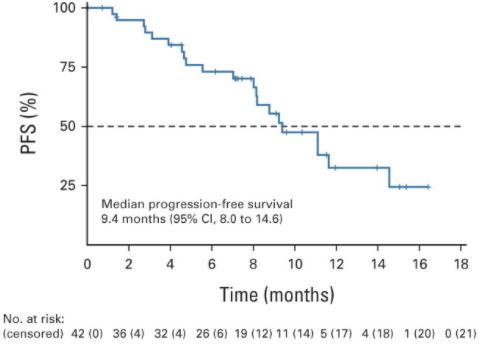
进展生存期和总生存期
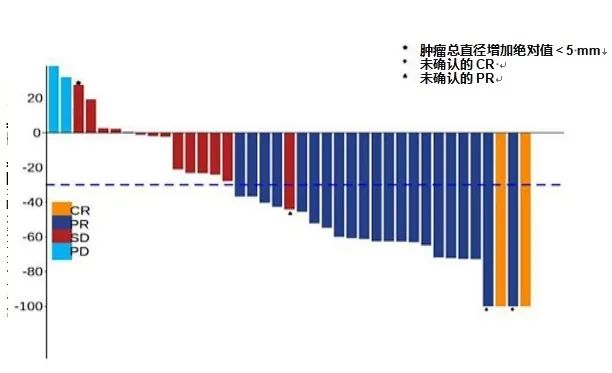
共招募了42位患者。客观缓解率为54.8%。在39位可评估疗效的患者中,客观缓解率为59.0%;疾病控制率达到了94.9%。中位无进展生存期为9.4个月。中位总生存期未达到。
85.8%的患者经历了治疗相关的副反应。最常见的治疗相关的副反应有甲状腺功能减退(33.3%)、天冬氨酸氨基转移酶水平升高(21.4%)和高血压(19.0%)。
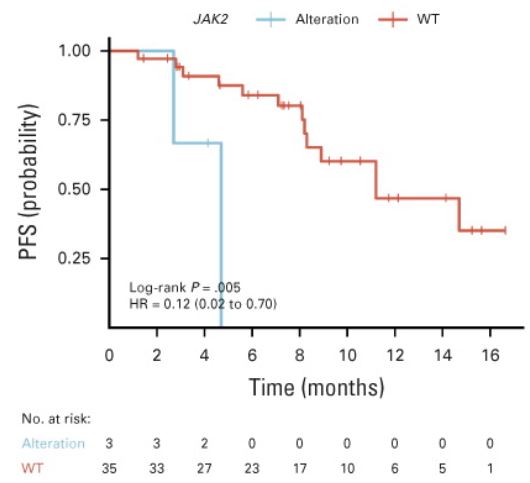
有无JAK2变异的患者的无进展生存期
携带PIK3CA、PI3K-AKT信号或KMT2D变异的患者拥有更高的客观缓解率,而携带STK11和(或)JAK2变异的患者的无进展生存期明显更短。
综上所述,该研究表明,信迪利单抗联合安罗替尼作为既往化疗失败的晚期宫颈癌患者的二线或晚线疗法是有效且安全的。
原始出处:
Qin Xu, et al. Efficacy and Safety of Sintilimab Plus Anlotinib for PD-L1–Positive Recurrent or Metastatic Cervical Cancer: A Multicenter, Single-Arm, Prospective Phase II Trial. Journal of Clinical Oncology. February 22, 2022. http://creativecommons.org/licenses/by-nc-nd/4.0/.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#信迪利单抗#联合#安罗替尼#治疗PD-L1阳性晚期#宫颈癌#
97
#Oncol#
36
#安罗替尼#
65
学习
52
#PD-L1#
39
#PD-L1阳性#
34
#宫颈#
37
#晚期宫颈癌#
32
学习了
50
靶免联合好像是趋势。
53