Neurology:美国**大学联合发现,遗传性阿尔茨海默病的风险因素
2021-02-01 Freeman MedSci原创
美国顶尖大学联合发现,遗传性阿尔茨海默病的风险因素
脑微出血(CMHs)或微出血(CMBs),即脑部小出血,常见于老年人,尤其是痴呆症患者。这些病变通常与:1)高血压有关,2)与阿尔茨海默病(AD)或脑淀粉样血管病(CAA)有关的血管β-淀粉样蛋白(Aβ),3)AD临床试验中的Aβ改变疗法()。
基线时CMHs的存在预示着在普通人群和AD中,将来会出现更多的CMHs。因此,在Aβ-修饰疗法的试验中,FDA建议监测CMHs并排除有5个或更多CMHs的参与者。
由于老年参与者通常具有混合病理,因此很难区分或确定这三个因素中的哪一个是CMHs的原因,尤其是在治疗试验中。评估一个年轻的队列,如具有显性遗传性AD(dominantly inherited AD, DIAD)的个体,血压相对正常且未接受治疗,可能有助于描述与AD独特相关的CMHs的自然发展过程。通过观察到DIAD患者在治疗试验中的变化,这会有助于能更好地理解CMHs的意义,
华盛顿大学的Nelly Joseph-Mathurin等人,利用了显性遗传性阿尔茨海默网络(DIAN)的数据,对参与者进行(amyloid-related imaging abnormalities,ARIA-H )评估,并对其进行长期跟踪,目的是确定与CMHs相关的临床风险,并确定发展出血性淀粉样蛋白相关影像异常(ARIA-H)的高风险个体的特征。
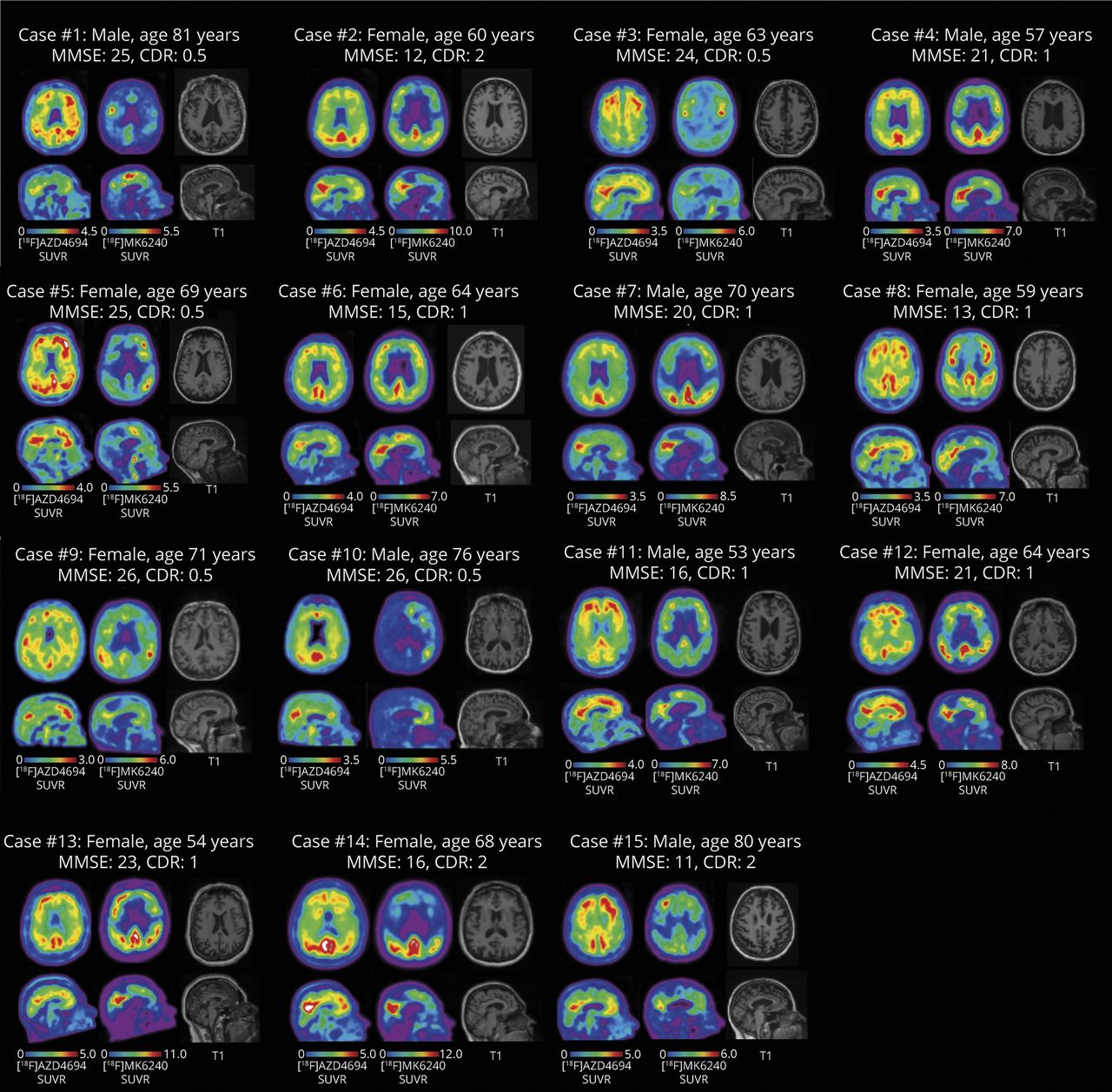
他们纳入了突变携带者(n=310)和非携带者(n=201),并进行神经影像学检查,包括梯度回波MR序列检测CMHs、神经心理学和临床评估。横断面和纵向分析评估了CMHs与神经影像学和疾病临床标志物之间的关系。
 结果显示,3%的非携带者和8%的携带者出现CMHs,主要位于脑叶区。和未出现CMH者相比,患有CMHs的携带者年龄较大,舒张压和Hachinski缺血评分较高,临床、认知和运动障碍更明显。
结果显示,3%的非携带者和8%的携带者出现CMHs,主要位于脑叶区。和未出现CMH者相比,患有CMHs的携带者年龄较大,舒张压和Hachinski缺血评分较高,临床、认知和运动障碍更明显。
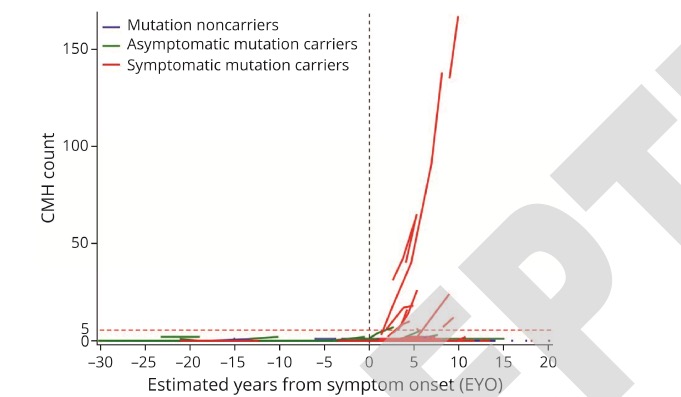
APOE-ε4状态与CMHs的流行或发生率无关。旧的或新发的CMHs可预测临床痴呆评级的更快变化。至关重要的是,随着时间的推移,存在两个或更多的CMHs与额外CMHs发展的显著风险相关(每年8.95±10.04)。
这个研究的重要意义在于,发现了和CMHs发生相关的因素。CMHs是DIAD潜在疾病过程的一部分,并与痴呆显著相关。接受药物治疗试验的参与者,可能会有ARIA-H作为并发症的风险,将CMHs的自然发生率与药物相关的CMHs分开可能是具有挑战性的。
原文出处;
Longitudinal Accumulation of Cerebral Microhemorrhages in Dominantly Inherited Alzheimer Disease; Nelly Joseph-Mathurin, Guoqiao Wang, et al.,
Neurology Jan 2021, 10.1212/WNL.0000000000011542; DOI: 10.1212/WNL.0000000000011542
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阿尔茨海#
25
#阿尔茨#
30
#Neurol#
32
#遗传性#
26
#阿尔茨海默#
23