亚硝酸钠制剂JAN101治疗COVID-19血管并发症
2020-08-07 Allan MedSci原创
生物制药公司JanOne已与世界领先的临床合同研究组织(CRO)CATO SMS达成协议。CATO SMS将协助JanOne推进JAN101的开发。
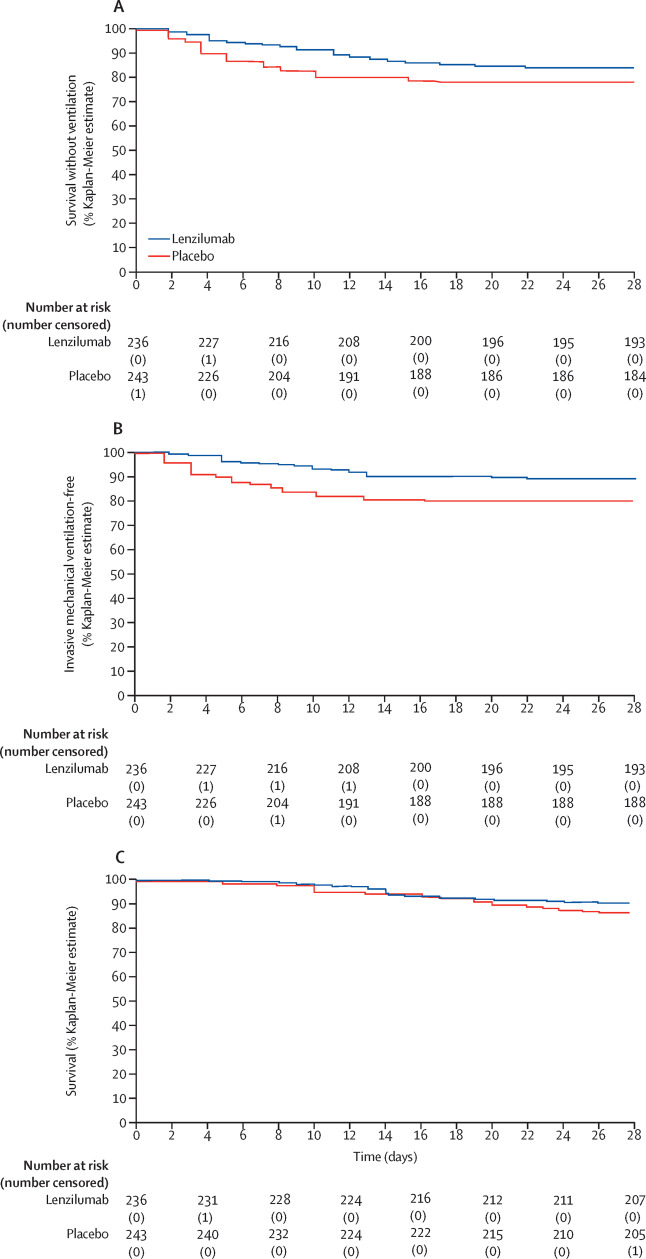
生物制药公司JanOne已与世界领先的临床合同研究组织(CRO)CATO SMS达成协议。CATO SMS将协助JanOne推进JAN101的开发。JAN101是一种口服、持续释放的亚硝酸钠制剂,可用于治疗COVID-19患者潜在的血管并发症,美国FDA已批准JAN101的研究性新药(IND)申请。此外,JAN101有望在2021年初进入IIb期临床试验,以治疗周围动脉疾病(PAD)。
最近发表在《新英格兰医学杂志》 上的一项研究表明,COVID-19引起的呼吸道并发症可能源于血管内皮细胞功能障碍。这意味着血管内皮细胞受到严重损害,并限制了人体将氧气携带到包括肺在内的人体主要器官的能力。先前的JAN101临床研究表明,JAN101可能对COVID-19患者有益。
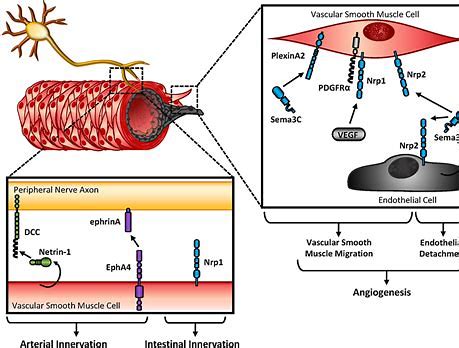
JanOne的首席科学官Tony Giordano博士称:“如果COVID-19是一种攻击内皮细胞的血管疾病,从而限制了向重要器官输送氧气的能力,那么我们的亚硝酸钠片剂JAN101可能会提供安全有效的治疗方法”。
CATO SMS将直接与JanOne领导团队和科学顾问委员会合作,CATO SMS法规事务高级副总裁MerriBeth Adams表示:“我们已经看到了COVID-19的毁灭性影响,以及它似乎对血管系统造成的严重损害。我们很高兴有机会与JanOne合作,并尽我们所能为COVID-19患者带来重要治疗机会”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
32
#亚硝酸钠#
22
#血管并发症#
26
阅读
82