梅氏微创消融术治疗心房颤动207例
2016-02-16 [db:作者] 中国胸心血管外科临床杂志CJCTCS
引用本文:马南, 姜兆磊, 陈飞, 等.梅氏微创消融术治疗心房颤动207例.中国胸心血管外科临床杂志, 2015, 22(11):996-999. [Ma N, Jiang ZL, Chen F, et al. Mei mini Mazeprocedure for 207 patients with atrial fib
心房颤动(房颤)是临床常见的心律失常之一。65岁以下人群的发病率1.9%,年龄超过65岁,其发病率约5%,当年龄超过80岁时,房颤的发病率则可达8%~l0%[1-2]。房颤时心房呈无序激动和无效收缩的房性节律,心房失去了有效的收缩功能,心室率不规则影响心室的充盈,使心排血量降低,尤其是心室率快者影响更大,因此可诱发心绞痛、心衰或晕厥等。更为严重的是,房颤时左心房特别是左心耳内易有血栓形成为导致栓塞和卒中的主要原因[3-4]。因此,控制心律(率)和抗凝是治疗房颤的两大原则[5]。目前治疗房颤方法有药物、导管、电复律、左心耳封堵和外科治疗等,哪种方法最为合适是我们面临的新问题。胸腔镜下房颤消融术不仅可以通过消融治疗房颤,还可以通过切除左心耳预防卒中,标本兼治,疗效日益受到肯定。梅举教授进一步改良了胸腔镜治疗房颤的术式—梅氏微创消融术[6-7]:在左心房顶部和后壁增加消融线从而提高了消融的成功率,将双侧胸壁的切口改为左侧胸壁的三个“小孔”,进一步减少手术创伤。我们应用该术式治疗房颤患者207例,临床效果良好。
1 资料与方法
1.1 临床资料
选自2010年10月至2014年2月房颤患者共207例,其中男111例、女96例,年龄 29~81 (58.9±14.8)岁。阵发性房颤98例,持续性房颤109例。参考由心律学会/欧洲心脏节律协会/欧洲心律协会发表的指南[8],患者均有心悸、胸闷等症状,房颤发作时查体可发现心尖部第一心音强弱不等,心律绝对不齐,脉搏短绌。所有患者术前均有心电图明确诊断。患者房颤病史(9.1±6.3)年,左心房直径(43.2±6.2) mm。术前心功能分级(NYHA) Ⅰ级63例,Ⅱ级110例,Ⅲ级28例,Ⅳ级6例。患者均签署手术知情同意书。手术适应证:药物治疗无效、或经过内科导管消融失败或有脑卒中或脑血栓史的房颤患者,左心室射血分数高于30%。心、肺手术史和左心房内径大于70 mm为相对禁忌证。
1.2 方法
1.2.1 手术方法 患者右侧卧位,术中常规采用选择性右肺单肺通气。术中经食管超声明确无左心房血栓。梅氏微创消融术技术要点如下:左胸第6肋间、第7肋间和第8肋间分别作25 mm-10 mm-10 mm的操作孔、辅助孔及腔镜孔,沿降主动脉前方1 cm处切开心包并悬吊,显露双侧肺静脉和左房后壁(图1A)。用双极射频消融钳分别进行双侧环肺静脉消融(图1B、图1C)和连接左右肺静脉的左心房顶部和后壁消融线(图1D)。使用切割闭合器切除左心耳。用AtriCure射频消融笔做左肺静脉到二尖瓣前瓣环的消融线(Dallas lesion)和左肺静脉至左心耳的消融线。三个环形消融加两条线性消融均在直视下完成。最后用消融笔消融Marshall韧带和肺静脉周围部分心外膜自主神经节。全部步骤完成后房颤仍不能终止者行电复律[9]。
1.2.2 围手术期处理 术后即给予胺碘酮 200 mg/d,术后3个月维持窦性心律的患者停用胺碘酮,不能维持窦性心律的患者以控制心室率为主。3个月后能维持窦性心律的患者停用抗凝药。不能维持窦性心律的患者参考CHA2DS2VASC评分和HAS-BLED评分选用华法林或阿司匹林抗凝。术后再发房颤在抗凝充分的条件下可予以直流电复律治疗。
1.2.3 随访 采用门诊复诊和电话等随访方式。为随访到术后的患者,我们设立了专值的随访人员,每例患者入院都详细登记地址,并留下至少3个联系电话(本人手机号、固定电话、儿女及亲属的电话)。术后1个月、3个月、6个月和12个月分别通过患者自觉症状及心电图、24 h动态心电图等检查,记录患者术后心律情况。术后3个月内为空白期,房颤发作不做统计。术后3个月随访中如发现房颤发生超过30 s,不管患者有无自觉症状,均视为房颤复发。
1.3 统计学分析
计量资料采用均数±标准差(X±s)表示。计数资料采用百分比表示。数据分析由SPSS18.0统计软件完成,P<0.05为差异有统计学意义。
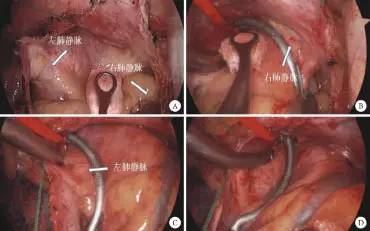
图1 胸腔镜下双侧肺静脉消融和环形消融
注:A为显露双侧肺静脉和左房后壁;B为消融右肺静脉;C为消融左肺静脉;D为从左下肺静脉至右上肺静脉的环形消融
2 结果
所有患者手术均顺利完成,无术中转为开胸手术,围手术期无患者死亡,无心脏起搏器置入。手术时间为(112.4±32.5) min。22例非阵发性房颤患者术后即刻行电复律。手术平均失血量较少,术中和术后均无输注血液制品。所有患者无严重并发症,平均住院时间(7.2±3.1) d。31例患者(15.0%)术后住院期间行电复律治疗,197例(95.1%)例患者出院时维持窦性心律。3例患者出院后因胸腔积液再次住院,行胸腔穿刺抽液和对症治疗后痊愈出院,5例患者伤口愈合不良。术后平均随访(24.2±8.9)个月,187(90.3%)例患者维持窦性心律,经24 h动态心电图证实,且患者均无心悸、胸闷等自觉症状。20例患者(8例阵发性房颤,12例持续性房颤)术后检查明确有复发房颤。阵发性房颤患者窦性心律转复率为91.8%(90/98),持续性房颤患者的窦性心律转复率为89.0%(97/109)。155例患者术后3个月停用胺碘酮并能维持窦性心律。所有患者术后3个月随访时行CT和超声心动图检查显示无肺静脉狭窄和左心房血栓。所有患者无卒中等脑血管不良事件发生。
3 讨论
房颤作为常见的心律失常之一,具有高致死率、高致残率,已被医患广泛重视[10]。目前主要的治疗策略是节律(率)治疗和抗凝治疗[11]。心律紊乱是最根本的病因,复律是房颤治疗的首选方式。复律治疗主要有药物复律、电复律、导管消融和外科手术等方法。药物复律成功率低,副作用大;导管消融一直未能解决其单次成功率低的问题[12-13]。传统外科手术虽然成功率高,但创伤大、术式复杂、术后并发症多而难以推广。由微创外科结合新型能量发展出的胸腔镜下房颤消融术单次成功率高,创伤小是现代外科治疗的主流术式[14-15]。
消融线的透壁、连续和完整是房颤复律治疗的关键[16-17]。胸腔镜下房颤消融术中使用的消融钳完成消融线是目前临床上保证消融线透壁和完整的最佳方法。各消融线在胸腔镜下直视完成,保证了各消融线的精确定位。这是胸腔镜下房颤消融术成功率高的主要原因。我们进一步研究发现以前的胸腔镜下房颤消融术仅能用消融钳完成环肺静脉消融,各线性消融还需消融笔来完成,这些消融线的透壁性难以保证。对于触发灶来源于肺静脉的房颤患者有较高的成功率,而对非肺静脉来源的房颤疗效欠佳。为了提高疗效,我们首先希望增加合适的左心房线性消融,像经典迷宫手术那样分割左心房组织、阻止大返折环的形成,其次增加的消融线也用消融钳完成,确保消融线的透壁质量[18]。梅氏微创消融术据此进行了创新。新的消融路线除了用消融钳完成环肺静脉消融,还增加了左心房顶部和后壁从左下肺静脉到右上肺静脉的环形消融线,并用消融钳保证了这些消融线的透壁质量,这在国内外微创外科消融房颤中是一个创新,因而提高了复律的成功率。本组中90.3%的患者可维持窦性心律,阵发性房颤患者窦性心律维持率为91.8%,持续性房颤患者的窦性心律维持率为89.0%,疗效较国外其他微创外科术式有显著提高[14-15]。
抗凝是房颤治疗的两大原则之一。按照指南推荐的CHA2DS2-VASC评分系统,大部分患者需要华法林或新型抗凝药的抗凝治疗。如何抗凝仍是治疗的棘手问题[19]。从药物选择方面,华法林的有效治疗窗窄,个体差异大;新型抗凝药的临床使用时间较短,安全性需进一步验证,费用昂贵。从患者自身方面,房颤患者往往合并高龄、高血压、糖尿病、卒中病史等,这些又是出血的危险因素。对于兼有高危出血风险的房颤患者,目前还没有合适的药物。房颤治疗的创始者James Cox提出在降低房颤脑卒中风险方面,机械性闭合左心耳比口服华法林更有效,应该被广泛应用[20]。左心耳切除是机械性闭合左心耳的可靠方法,左心耳切除后能在不服用抗凝药的情况下减少左房血栓的形成进而降低栓塞[21]。左心耳切除是我们术式中重要的组成部分,除了可以去除左心耳上的异位触发灶提高复律的成功率,更可以有效地减少血栓的形成,预防卒中,同时避免服用抗凝药的出血风险。本组患者均顺利切除了左心耳,同时我们选择性地降低了部分术后患者的抗凝强度和抗凝时间,目前随访数据显示本组患者尚无卒中和出血等脑血管不良事件发生。
梅氏微创消融术避免体外循环和心脏停跳,保持胸廓的完整性,只须左侧胸壁的三个孔洞即能完成手术,是真正意义上的“微创”术式。与一般心脏外科手术相比,该术式在全胸腔镜下进行,心外科医师需经过相关腔镜手术的训练。与其他胸腔镜下房颤消融的术式相比,该术式在操作上避免双侧胸腔切口,可有助手协助,全部步骤均在直视下进行,安全可靠。总的来说,梅氏微创消融术操作简便,手术时间短;手术创伤小,术后患者恢复快,手术治愈率高,是治疗房颤安全、有效的方法。
参考文献
1 Zhou Z, Hu D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland china. J Epidemiol, 2008, 18 (5): 209-216.
2 Martinez C, Katholing A, Wallenhorst C, et al. Increasing incidence of non-valvular atrial fibrillation in the UK from 2001 to 2013. Heart, 2015, Aug 25. doi: 10.1136/heartjnl-2015-307808.
3 McCabe PJ, Rhudy LM, Chamberlain AM, et al. Fatigue, dyspnea, and intermittent symptoms are associated with treatment-seeking delay for symptoms of atrial fibrillation before diagnosis. Eur J Cardiovasc Nurs, 2015 Aug 28. pii: 1474515115603901.
4 Alli O, Holmes DR Jr. Left atrial appendage occlusion for stroke prevention. Curr Probl Cardiol, 2012, 37(10): 405-441.
5 January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation, 2014, 130(23): 2071-2104.
6 Mei J, Ma N, Ding F, et al. Complete thoracoscopic ablation of the left atrium via the left chest for treatment of lone atrial fibrillation. J Thorac Cardiovasc Surg, 2014, 147(1): 242-246.
7 马南, 梅举, 丁芳宝, 等. 左胸径路微创外科治疗孤立性房颤. 中华胸心血管外科杂志, 2013, 29(11): 692-693.
8 Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the managementof atrial fibrillation: the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur Heart J, 2010, 32(9): 2369-2429.
9 Ma N, Ding F, Jiang Z, et al. Totally endoscopic ablation of left atrium via left chest for lone atrial fibrillation. Innovations (Phila), 2012, 7(5): 382-384.
10 Scherr D, Jais P. Atrial fibrillation: AF prognosis and treatment--the European perspective. Nat Rev Cardiol, 2014, 11(12): 689-690.
11 Rolf S, Kornej J, Dagres N, et al. What can rhythm control therapy contribute to prognosis in atrial fibrillation ? Heart, 2015, 101(11): 842-846.
12 Lewalter T, Ibrahim R, Albers B, et al. An update and current expert opinions on percutaneous left atrial appendage occlusion for stroke prevention in atrial fibrillation. Europace, 2013, 15(5): 652-656.
13 Crandall MA, Bradley DJ, Packer DL, et al. Contemporary manage-ment of atrial fibrillation: update on anticoagulation and invasive management strategies. Mayo Clin Proc, 2009, 84(7): 643-662.
14 Wolf RK, Schneeberger EW, Osterday R, et al. Video-assisted bilateral pulmonary vein isolation and left atrial appendage exclusion for atrial fibrillation. J Thorac Cardiovasc Surg, 2005, 130(3): 797-802.
15 Yilmaz A, Geuzebroek GS, Van Putte BP, et al. Completely thoracoscopic pulmonary vein isolation with ganglionic plexus ablation and left atrial appendage amputation for treatment of atrial fibrillation. Eur J Cardiothorac Surg, 2010, 38(3): 356-360.
16 Andrade JG, Macle L. Improving ablation strategies for the treatment of atrial fibrillation. Expert Rev Med Devices, 2014, 11(1): 77-88.
17 Benussi S, Nascimbene S, Calori G, et al. Surgical ablation of atrial fibrillation with a novel bipolar radiofrequency device. J Thorac Cardiovasc Surg, 2005, 130(2): 491-497.
18 Wisser W, Seebacher G, Fleck T, et al. Permanent chronic atrial fibrilltion: is pulmonary vein isolation alone enough. Ann Thorac Surg, 2007, 84(4): 1151-1157.
19 Gallagher AM, Setakis E, Plumb JM, et al. Risks of stroke and mortality associated with suboptimal anticoagulation in atrial fibrillation patients. Thromb Haemost, 2011, 106(5): 968-977.
20 Cox JL. Mechanical closure of the left atrial appendage: is it time to be more aggressive? J Thorac Cardiovasc Surg, 2013, 146(5): 1018-1027.
21 Ohtsuka T, Ninomiya M, Nonaka T, et al. Thoracoscopic stand-alone left atrial appendectomy for thromboembolism prevention in nonvalvular atrial fibrillation. J Am Coll Cardiol, 2013, 62(2): 103-107
引用本文:马南, 姜兆磊, 陈飞, 等.梅氏微创消融术治疗心房颤动207例.中国胸心血管外科临床杂志, 2015, 22(11):996-999. [Ma N, Jiang ZL, Chen F, et al. Mei mini Mazeprocedure for 207 patients with atrial fibrillation. Chin J Clin ThoracCardiovasc Surg, 2015, 22(11): 996-999. ]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#微创#
22
#消融#
24
#消融术#
28
#消融术#
39
#心房#
0