Clin Cancer Res:Adavosertib联合各种化疗药治疗原发铂耐药的卵巢癌、输卵管癌、腹膜癌
2022-01-07 Nebula MedSci原创
Adavosertib联合各种化疗药治疗原发铂耐药的卵巢癌、输卵管癌、腹膜癌具有初始的治疗活性
Adavosertib (AZD1775) 是酪氨酸激酶WEE1的小分子抑制剂,具有潜在的抗肿瘤活性。本研究旨在评估Adavosertib联合四种原发性铂类耐药性卵巢癌常用的化疗药物治疗原发性铂类耐药性卵巢癌的疗效、安全性和药代动力学。
这是一项开放标签的、四臂的、多中心的II期临床试验,于2015年1月至2018年1月期间,招募了94位组织学或细胞学确诊的具有可测量病灶的上皮性卵巢癌、输卵管癌或腹膜癌患者。受试患者被分成了6个队列,每天接受175mg-225mg的Adavosertib(口服胶囊,吃2天、停5天,或吃3天、停4天)联合吉西他滨、紫杉醇、卡铂或聚乙二醇化脂质体阿霉素。主要终点是总缓解率。
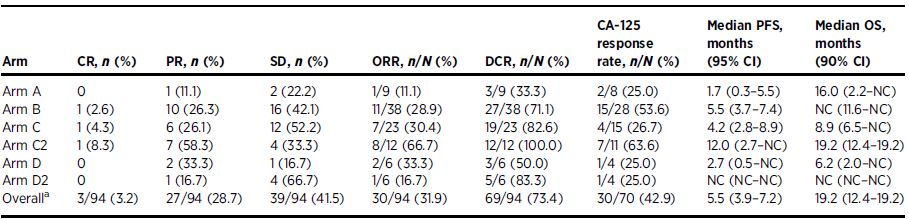
各治疗组的缓解情况
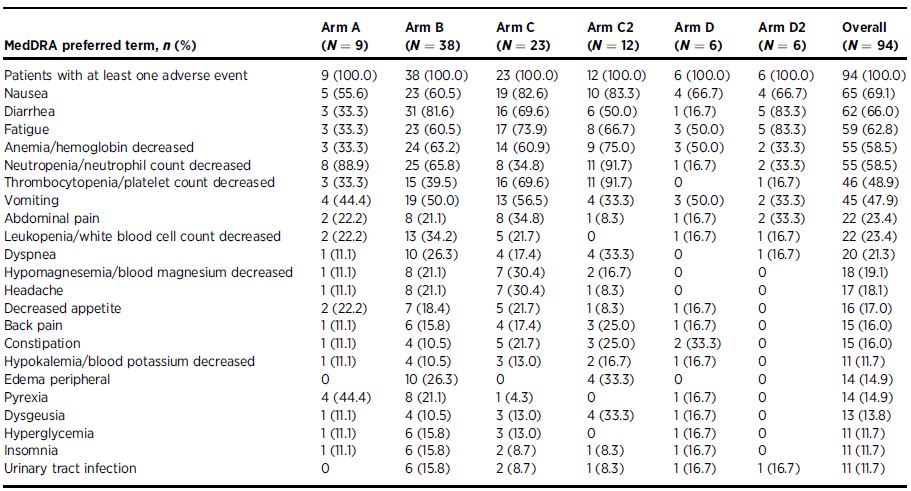
在94位患者中,有3位(3%)获得了经验证的完全缓解,27位(29%)获得了客观缓解。缓解率最高的队列是卡铂联合Adavosertib组,缓解率和疾病控制率分别是66.7%和100%,中位无进展生存期是12.0个月。最长的缓解持续时间在紫杉醇队列(12.0个月)。所有队列最常见的3级及以上的副反应有中性粒细胞减少症(47.9%)、贫血(33.0%)、血小板减少症(31.9%)和腹泻与呕吐(10.6%)。
最常见的副反应
总之,Adavosertib在该研究的受试患者人群中与化疗药物联用时展现出了初始的治疗活性。最有希望的治疗组合是在第1-3、8-10 和15-17天每天予以两次Adavosertib 225 mg 加上每21天一次卡铂。但是,该联合方案的血液学毒性比卡铂单药治疗更频繁,需要进一步研究以优化剂量、用药方案和支持药物。
原始出处:
Kathleen N. Moore, et al. Adavosertib with Chemotherapy in Patients with Primary Platinum-Resistant Ovarian, Fallopian Tube, or Peritoneal Cancer: An Open-Label, Four-Arm, Phase II Study. Clin Cancer Res January 1 2022 28 (1) 36-44; DOI:10.1158/1078-0432.CCR-21-0158
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#铂#
38
#输卵管#
33
#ADA#
43
#腹膜癌#
41
#输卵管癌#
36
#化疗药#
32
#腹膜#
36