PARTNER队列A:高危主动脉狭窄患者,经导管主动脉瓣植入(TAVI)治疗,不劣于传统主动脉瓣置换手术(AVR)
2011-04-09 MedSci原创 MedSci原创
2011年4月4日,备受关注的PARTNER研究队列A的结果在美国心脏学会2011年科学年会上揭晓。该研究显示,在高危主动脉狭窄患者中,经导管主动脉瓣植入(TAVI)治疗,不劣于传统主动脉瓣置换手术(AVR)的效果。 主动脉狭窄由于动脉瓣黏连导致,每年全美多达9%的65岁以上人群罹患该病,发病率随年龄的增长而逐步增加。目前主要治疗方案为开胸手术。 研究共入选了699例高危老
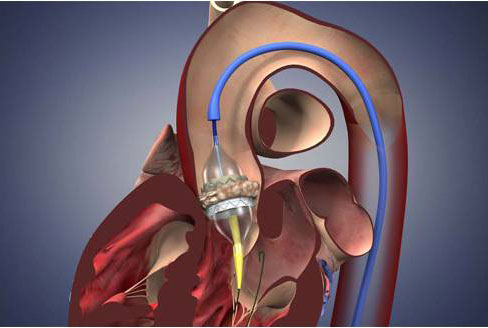
2011年4月4日,备受关注的PARTNER研究队列A的结果在美国心脏学会2011年科学年会上揭晓。该研究显示,在高危主动脉狭窄患者中,经导管主动脉瓣植入(TAVI)治疗,不劣于传统主动脉瓣置换手术(AVR)的效果。
主动脉狭窄由于动脉瓣黏连导致,每年全美多达9%的65岁以上人群罹患该病,发病率随年龄的增长而逐步增加。目前主要治疗方案为开胸手术。
研究共入选了699例高危老年主动脉狭窄患者,随机分配至26个医疗中心进行TAVR或主动脉瓣置换手术治疗,患者平均年龄84.1岁,其中TAVR组348名患者,AVR组350名患者。研究终点包括一年内任何原因死亡(主要终点)、卒中与大血管出血事件。
与AVR组相比,TAVI组30天内全因死亡率更低,(3.4%对6.5%),症状改善程度更高,研究进行1年时,两组患者有明显差异(24.2%对 26.8%)。在次要终点结果中,与手术组相比,TAVI组30日内(3.8%对2.1%)及1年内(5.1%对3.2%)大卒中发生率均更高。30日内大血管并发症更多(11.0%对3.2%),然而大出血发生率更低(9.3%对19.5%),房颤患者新发心律不齐的比例也更低(8.6%对 16.0%)。TAVI 组瓣膜返流发生率更高。
研究主要负责人、哥伦比亚大学纽约长老会医院的Craig R. Smith教授表示,研究结果充分证实,对于那些高危主动脉狭窄患者,TAVI不失为传统主动脉瓣置换手术的一种优秀替代治疗方案。今后尚需进一步观察TAVI在中危患者中的作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AVR#
28
#经导管主动脉瓣植入#
24
#置换#
38
#PARTNER#
33
#主动脉狭窄#
37
#主动脉瓣#
23
#ART#
32
#主动脉#
24
#动脉狭窄#
26
#经导管#
33