JCEM:绝经后骨质疏松症,双药联合优于单药(DATA-HRpQCT研究)
2016-03-28 Seven L MedSci原创
近期发表在J Clin Endocrinol Metab的研究表明,治疗绝经后骨质疏松症时,联合使用狄诺塞麦和特立帕肽将优于单药治疗,主要表现在臀部和脊柱骨矿物质密度的增加。研究者对94名绝经后骨质疏松症女性进行了一项随机对照试验,探究联合治疗2年对患者骨骼微结构和骨强度的影响。研究者将患者随机分为每日皮下注射特立帕肽20μg组、每6个月皮下注射狄诺塞麦60μg组、两种药物联合治疗组,3组治疗时间
近期发表在J Clin Endocrinol Metab的研究表明,治疗绝经后骨质疏松症时,联合使用狄诺塞麦和特立帕肽将优于单药治疗,主要表现在臀部和脊柱骨矿物质密度的增加。
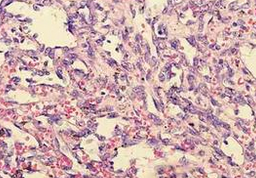
研究者对94名绝经后骨质疏松症女性进行了一项随机对照试验,探究联合治疗2年对患者骨骼微结构和骨强度的影响。研究者将患者随机分为每日皮下注射特立帕肽20μg组、每6个月皮下注射狄诺塞麦60μg组、两种药物联合治疗组,3组治疗时间均为2年。
研究数据显示,桡骨和胫骨总的容积骨密度(vBMD)、桡骨骨小梁vBMD和胫骨皮质vBMD在联合治疗组高于单药治疗组(P值均<0.002)。联合治疗组胫骨皮质厚度增加更多(8.1±4.3%)(相比单药治疗组)(P<0.001)。特立帕肽组患者在24个月治疗过程中,桡骨和胫骨皮质骨松化进行性增加,其他两组患者皮质骨松化稳定(P值均<0.001)。此外,所有小组胫骨小梁vBMD增加相似,不过桡骨vBMD方面,联合治疗与单药治疗组相比,增加更多(所有对比,P<0.01)。
研究结果表明,使用狄诺塞麦和特立帕肽联合治疗两年,可显著改善骨微结构和骨强度,疗效优于单药治疗,尤其是骨密度。
原始出处:
Tsai JN,Uihlein AV,Burnett-Bowie SM,et al.Effects of Two Years of Teriparatide, Denosumab, or Both on Bone Microarchitecture and Strength (DATA-HRpQCT study).J Clin Endocrinol Metab 2016 Mar 10;:jc20161160[Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
36
#JCEM#
25
#绝经#
24
#ATA#
37
#绝经后骨质疏松症#
34
#骨质#
33
#绝经后#
21
值得学习
134
深入研究
94