Radiology:扩散加权MRI成像,使VHL相关性肾透明细胞癌的个性化检测成为可能
2021-06-10 shaosai MedSci原创
Von Hippel–Lindau(VHL)病是一种多系统遗传性癌症综合征,可并发中枢神经系统和视网膜血管母细胞瘤、胰腺及肾脏囊肿、神经内分泌肿瘤,附睾囊腺瘤以及实性或囊性ccRCCs.
 Von Hippel–Lindau(VHL)病是一种多系统遗传性癌症综合征,可并发中枢神经系统和视网膜血管母细胞瘤、胰腺及肾脏囊肿、神经内分泌肿瘤,附睾囊腺瘤以及实性或囊性透明细胞型肾细胞癌(ccRCCs)。尽管肾细胞癌和中枢神经系统血管母细胞瘤的治疗进展改善了VHL病患的长期预后,但肾脏肿瘤仍是主要的死亡原因。
Von Hippel–Lindau(VHL)病是一种多系统遗传性癌症综合征,可并发中枢神经系统和视网膜血管母细胞瘤、胰腺及肾脏囊肿、神经内分泌肿瘤,附睾囊腺瘤以及实性或囊性透明细胞型肾细胞癌(ccRCCs)。尽管肾细胞癌和中枢神经系统血管母细胞瘤的治疗进展改善了VHL病患的长期预后,但肾脏肿瘤仍是主要的死亡原因。
由于较小的肿瘤很少发生转移,因此为了最大程度地减少不必要的手术操作,临床上常规建议对患者进行主动监视,直到肿瘤的最大直径达到3 cm。另外,患有VHL疾病的患者经常在一个时间点患有许多肾肿瘤。因此,建立一种评估患者体内肾脏内多个肿瘤生长动力学变化的方法可以提高对具有最高生长速率的肿瘤的识别和追踪,使得在最佳时间点进行手术干预成为可能。
MRI是监测VHL相关肾肿瘤的主要手段,使用诸如扩散加权(DW)等序列可提高肿瘤特征的识别和整体患者的治疗。现阶段,DWI序列已常规应用于肿瘤成像以检测和表征肿瘤,同时进行治疗反应的预测和监测。然而据我们所知,尚未有探讨ADC值与肾肿瘤生长之间的纵向关系的相关研究。
近日,发表在Radiology杂志的一项研究探讨了量化为ADC的MRI扩散受限程度对VHL相关ccRCC的增长率的预测价值,为患者治疗方案的个性化制定提供参考依据,从而有助于减少不必要的筛查和优化床干预。
本研究回顾性分析了2014年11月至2017年10月期间接受肿瘤手术切除的VHL疾病患者。通过两名阅读者分别在CT肾实质期和扩散加权MRI图像上进行分割,计算两个时间点ccRCC体积的变化和基线时的表观扩散系数(ADC)。用组内相关系数评价读者之间的一致性。使用重复测量相关性研究ADC(直方图参数)和肿瘤大小基线与生长速率和体积倍增时间(VDT)之间的关系。回顾具有最高相关性的ADC参数和肿瘤大小在基线时的预测性能,以根据VDT(≤1年或>1年)区分肿瘤。
本研究评估了46例患者(平均年龄46岁±7岁[标准差];25名女性)的共100例ccRCCs。读者间的一致性导致平均ADC、基线肿瘤体积和随访肿瘤体积的平均κ得分分别为0.89、0.82和0.93。ADC百分位与肿瘤生长速率呈负相关,与VDT呈正相关。ADC值越低,相关性越强。第25百分位ADC与肿瘤生长速率(ρ = -0.52, P < .001)和VDT (ρ = 0.60, P < .001)相关性最强,且能够预测VDT(≤1年或>1年),受试者作特征曲线下面积为0.86(敏感性,67%;特异性,89%)(P < .001)。

图1 55岁,男性,VHL合并肾透明细胞癌。(a, b)轴位增强CT肾实质期图像显示,基线时肿瘤为7.4 cm3 (a), 125天时肿瘤增长至9.1 cm3 (b)。(c)基线时肿瘤轴位表观扩散系数(ADC)图和(d)相应的直方图百分位分析。
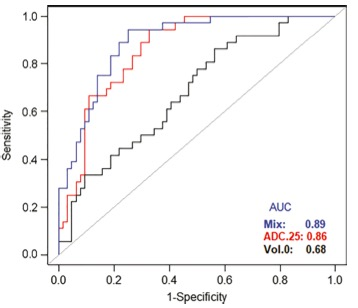
图2 该图显示了使用基线(黑色)、第25百分比表观扩散系数(ADC25%)(红色)和两者组合(蓝色)区分体积倍增时间≤1年或>1年肿瘤的受试者工作特征曲线。
本研究表明,基线时表观扩散系数值使得鉴别增长速度明显的肾透明细胞癌肿瘤成为可能。本研究的发现避免了临床对VHL患者的低风险肾肿瘤进行不必要的密集监测,并将注意力集中在快速生长和转移的高风险肿瘤上,为制定个性化的临床治疗方案提供了一个有价值的影像学工具。
原文出处:
Faraz Farhadi,Moozhan Nikpanah,Anna K Paschall,et al.Clear Cell Renal Cell Carcinoma Growth Correlates with Baseline Diffusion-weighted MRI in Von Hippel-Lindau Disease.DOI:10.1148/radiol.2020191016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#透明细胞癌#
28
#相关性#
19
#细胞癌#
23
#VHL#
39