HER-2与抗-EGFR治疗——HER-2与转移性结直肠癌(二)
2017-08-04 佚名 肿瘤资讯
HER-2与抗-EGFR治疗——HER-2与转移性结直肠癌(二)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















HER_2与转移性结直肠癌.
97
#转移性#
51
#结直肠#
34
#HER-2#
43
#GFR#
35
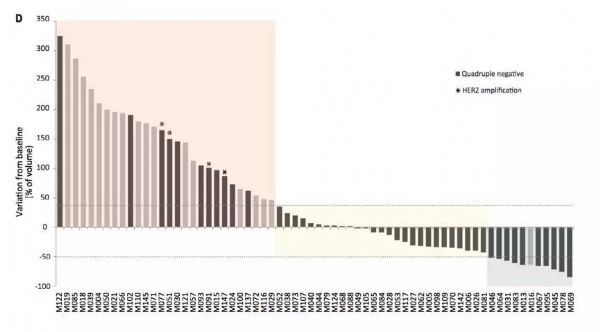
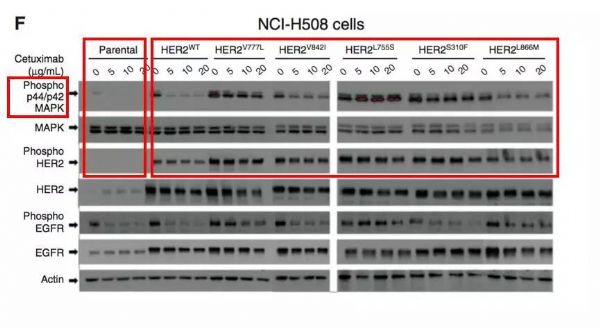
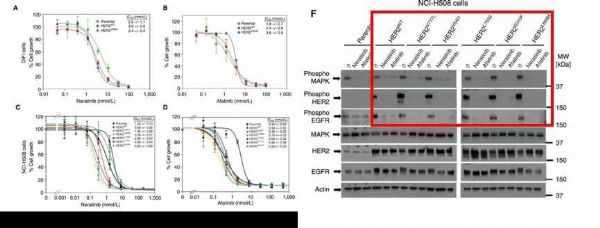
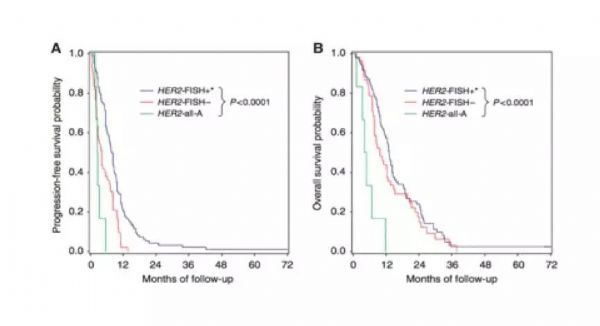
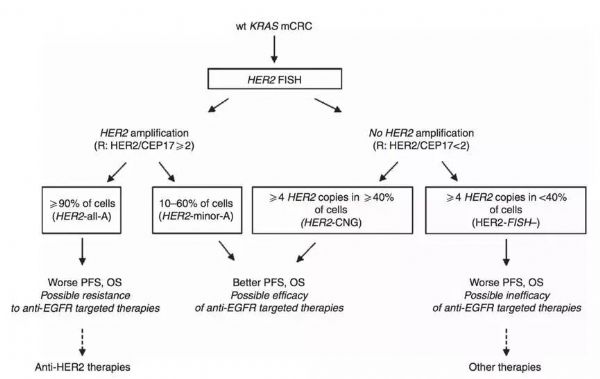
HER2强阳性和HER2阴性表达的患者,CET反应最差;HER2强阳性的患者,长期生存最差,而生存最好的反而是HER2弱阳性表达的患者。
81
非常好的文章,学习了,很受益
0
学习了新知识
83
学习了,涨知识
78