Neurology:ENCT随机对照试验:脑动脉瘤血管内治疗后发生的医源性脑梗死与术后认知、临床随访指标差异相关
2022-03-08 Naomi MedSci原创
近日,研究人员对接受颅内动脉瘤血管内修复治疗的患者进行了ENCT随机对照试验。研究发现医源性脑梗死与不同量表评估下的术后(1-4天)、30天结局的细微差异有关,早期的功能障碍与后期差异相关。
外科手术或血管内治疗引起的医源性脑梗死通常只在磁共振弥散加权成像(DWI)序列上可见。这些脑梗死通常是“沉默的”,并没有明显的症状。虽然患者不会定期接受手术后的脑MRI检查,但无症状的医源性梗死很常见。在接受神经介入手术(如脑动脉瘤弹簧圈)后,风险更高,发生在49-67%的患者,而接受其他非心脏手术的患者为7-10%。然而,医源性梗死的临床意义尚不确定。
越来越多的证据表明,医源性脑梗塞可能会导致持久的脑损伤。组织学上,它们代表类似于症状性卒中的神经元坏死。虽然一些在系列成像上得到解决,但只有少数真正消失。动物研究已经将这些梗死与未来的卒中和行为异常联系在一起。关于自发性(非医源性)无症状脑梗死的相关文献表明,细微的临床缺陷,如精细运动障碍、头晕、视野缺陷和抑郁症状(明显无症状的梗死),这些患者随后发生重大卒中的风险更高。在鹿特丹和AGES-雷克雅未克的前瞻性队列研究中,无症状的自发性脑梗死也与3-5年后认知能力下降和痴呆的风险增加有关。虽然这些观察表明医源性脑梗死也可能导致认知能力下降,这一点在接受手术的患者中仍有待证明,因为从机制上讲,医源性脑梗死可以在没有脑小血管疾病(CSVD)或心血管疾病的情况下发生,这是自发性发展的基础。
2016年对8项研究(281名患者)进行的荟萃分析得出结论,治疗未破裂的脑动脉瘤不会影响一般认知功能,但这些研究并没有通过脑MR对医源性梗死完成一致性的评估。到目前为止,关于医源性梗死临床后遗症最令人信服的证据来自NeuroVision前瞻性队列研究,该研究发现,与没有围手术期隐匿性卒中的老年患者(≥65岁)相比,一年后在使用蒙特利尔认知评估和数字符号替代测试进行评估,患有围术期静止性卒中的老年患者(n=78/1,114)围手术期神志不清和认知能力下降的风险更高。然而,只有大约四分之一的患者进行了脑MRI检查。重要的是,以前的研究没有检查医源性梗死的数量和临床结果之间的关系。像MoCA这样的短期测试对术后细微变化的敏感度也可能有限。
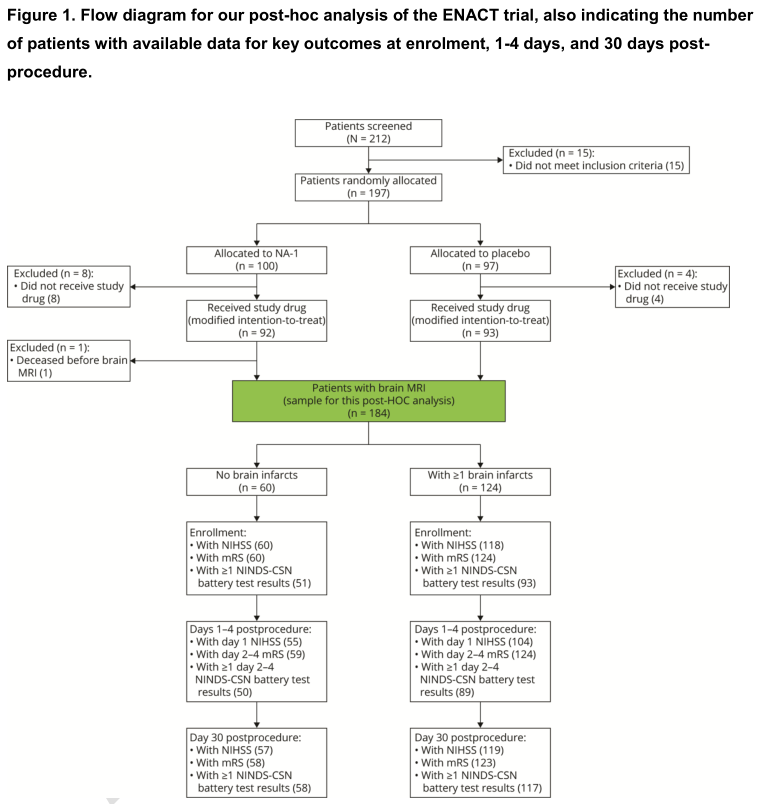
如果没有令人信服的临床后果证据,医源性脑梗死可能会被误解为不重要的问题。考虑到神经介入手术的数量不断增加(美国每年超过30万次血管造影)。近日,研究人员对接受颅内动脉瘤血管内修复的患者进行了ENCT随机对照试验(评估动脉瘤血管内治疗中的神经保护),研究了医源性梗死与预后的关系,并假设医源性梗死患者的术后结果会更差,而且梗死数量越多,这些结果就越差。
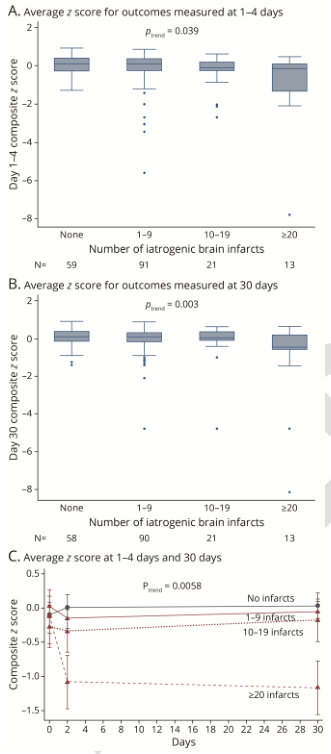
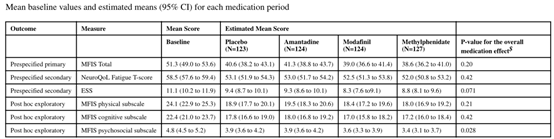
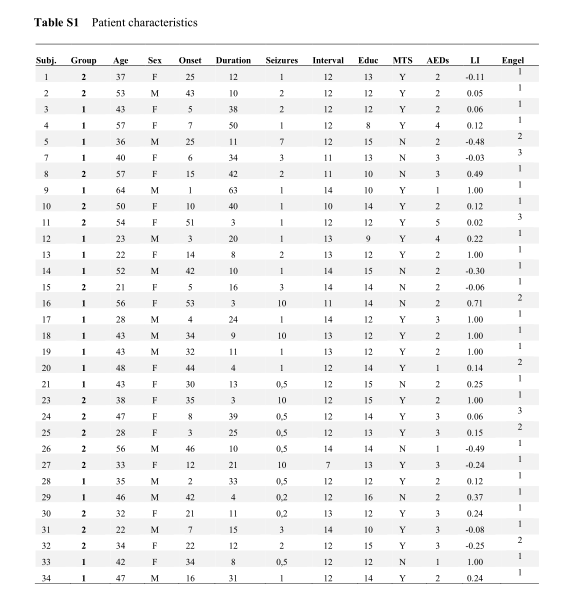
在这项事后分析中,使用多变量模型来评估DWI上医源性梗死的存在和数量与术后1-4天和30天的神经损害(美国国立卫生研究院卒中评分[NIHSS])、功能状态(改良的Rankin评分[MRS])、认知和神经精神结局(30分钟测试组合)的相关性。还使用分位数回归将梗死数量与Z分数衍生的综合结果评分联系起来。
- 184例患者(中位年龄56岁,IQR50~64岁)中,术后DWI病变124例(67.4%),中位病变数4(IQR2~10.5)。
- 去甲肾上腺素治疗与较少的医源性梗死有关,但总体上没有显着的临床治疗效果。
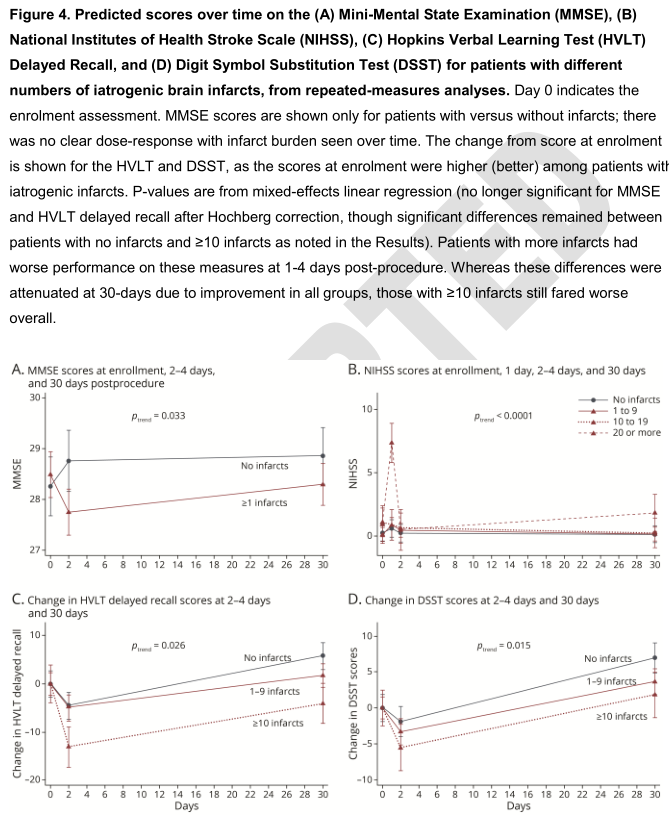
- 梗死患者在2-4天的简易智力状态检查得分较低(中位数28vs29,调整系数[coef]:-1.11,95%CI-1.88to-0.34,p=0.005)。
- 病灶计数越多,第1天的NIHSS评分越差(≥为1.07,1.02-1.12,p=0.009),第2-4天的MRS(调整后的共同优势比[AOR]:1.05,1.011.09,p=0.005)和第2-4天的MMSE评分(COEF:-0.07,-0.13to-0.003,p=0.040)较差。
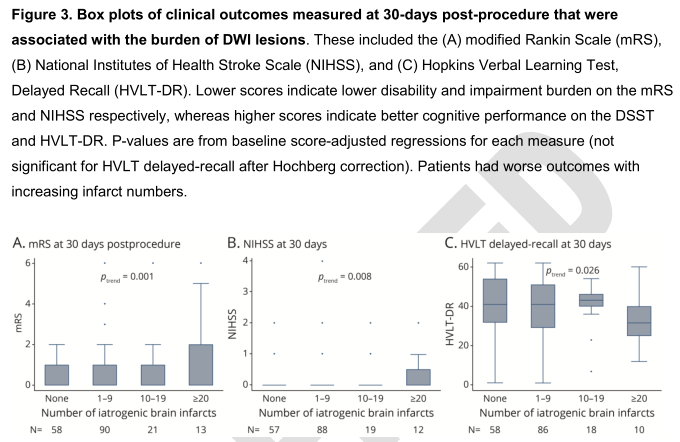
- 在30天时,梗死数目仍然与更差的MRS(AOR:1.04,1.01-1.07,p=0.016)和霍普金斯语言学习测验延迟回忆分数(ACEF:-0.21,-0.39to-0.03,p=0.020)有关。梗死患者30天数字符号替代试验得分较低(COEF:-3.73,-7.36~0.10,p=0.044)。
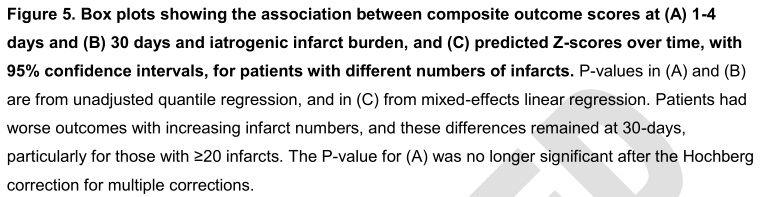
- 病变数量越多,1-4天和30天的综合预后评分越差(30天系数:-0.12,95%CI-0.21to-0.03,p=0.008)。
- 在梗死组中,第1天的NIHSS、第2-4天的MRS与30天的NIHSS、DSST、HVLT和MRS评分相关,而第2-4天的MMSE与30天的NIHSS和DSST评分相关(Spearman-Rho:0.47p=0.001)。
在这个中年队列中,医源性脑梗死与不同量表评估下的术后(1-4天)、30天结局的细微差异有关,早期的功能障碍与后来的差异相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Neurol#
31
#对照#
31
#对照试验#
45
#随机对照试验#
0
#脑梗#
43
#脑动脉瘤#
39