Am J Transl Res:研究揭示当归补血汤治疗糖尿病肾病的机制
2017-09-06 MedSci MedSci原创
当归补血汤(DBT)是一种中医汤剂,研究已经证实其可有效治疗糖尿病肾病(DN)。在这项研究中,研究人员探讨了DBT在DN治疗中的潜在机制。研究人员通过DBT为小鼠灌胃制备含血清的DBT。用ELISA检测细胞培养液中的纤维连接蛋白(FN)、层粘连蛋白(LN)、Ⅳ型胶原(COL IV)和TGF-β1蛋白的水平。采用qRT-PCR和Western blotting测定相关分子的mRNA及蛋白的表达。MT
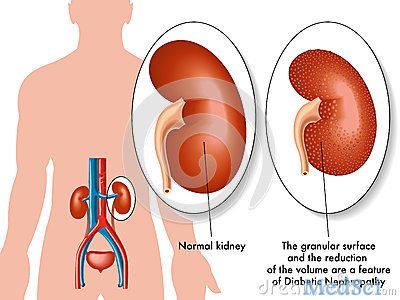
当归补血汤(DBT)是一种中医汤剂,研究已经证实其可有效治疗糖尿病肾病(DN)。在这项研究中,研究人员探讨了DBT在DN治疗中的潜在机制。
研究人员通过DBT为小鼠灌胃制备含血清的DBT。用ELISA检测细胞培养液中的纤维连接蛋白(FN)、层粘连蛋白(LN)、Ⅳ型胶原(COL IV)和TGF-β1蛋白的水平。采用qRT-PCR和Western blotting测定相关分子的mRNA及蛋白的表达。MTT法检测细胞增殖。
结果显示,DBT对高糖(HG)诱导的细胞增殖和肾小球系膜细胞(MC)累积的细胞外基质(ECM)产生负面影响。进一步的研究表明,DBT可减少PVT1启动子位点组蛋白H3的乙酰化水平以促进PVT1下调,同时伴随着TGF-β和c-myc的表达减少。此外,PVT1过表达可显著增强细胞活力,并促进TGF-β1基因的表达水平。此外,PVT1过表达可显著逆转DBT抑制高糖诱导的细胞活力和细胞外基质积聚,同时还可去除DBT对TGF-β1和c-myc表达的影响。
总之,该研究结果表明,通过下调PVT1,DBT可抑制TGF-β1和c-myc的表达,从而减弱MCS的过度增殖和ECM的累积。
原始出处:
Rui Zhang, Jinbo Li, Tao Huang, Xiuge Wang. Danggui buxue tang suppresses high glucose-induced proliferation and extracellular matrix accumulation of mesangial cells via inhibiting lncRNA PVT1. Am J Transl Res. 2017; 9(8): 3732–3740. Published online 2017 Aug 15.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Transl#
27
#TRA#
44
继续学习.
72
非常好的文章.学习了
66
学习了受益匪浅
74
学习了.谢谢!
59
中药中医博大精深
62