适合筛选前列腺根治性切除术患者的新评分系统
2021-09-05 盖伦 MedSci原创
多参数磁共振成像(mpMRI)在前列腺癌诊断中的作用逐渐显现,这种成像方式目前被国际指南推荐用于前列腺癌的诊断路径。此外,mpMRI可以帮助医生识别哪些患者适合根治性前列腺癌手术。
在过去的十年中,多参数磁共振成像(mpMRI)在前列腺癌(PCa)诊断中的作用逐渐显现,这种成像方式目前被国际指南推荐用于前列腺癌的诊断。此外,mpMRI可以帮助医生识别在根治性前列腺切除术(RP)中更有可能产生较差预后的患者。
《欧洲泌尿外科杂志》在近日刊登了一篇基于临床特征和mpMRI的评分系统并且优于目前的风险评估系统,有利于临床医生筛选出适合RP患者。
方法
在2014年至2020年期间,2819名患者在7个转诊中心接受了MRI-靶向活检和随后的RP合并扩大盆腔淋巴结清扫。患者均没有接受术前雄激素剥夺治疗。所有患者在前列腺活检前均接受mpMRI检查,使用1.5或3-T扫描仪。根据欧洲泌尿生殖学会放射学指南,成像方案包括多平面t2加权图像、弥散加权图像、动态对比增强mpMRI和脂肪抑制的t1加权图像。
术前PSA、临床分期(根据主治泌尿科医生的直肠指诊(DRE))、前列腺体积测量和影像学资料(PI-RADS评分、囊外扩张[ECE]、精囊浸润[SVI]、mpMRI指标病变最大直径(PI-RADS评分最高的病变或相同PI-RADS评分的病变直径最大的病变)。根据这些指标经过筛选后构建模型如图1

图1 预测根治性前列腺切除术3年随访后生化复发风险的诺莫图
BCR =生化复发;ECE =囊外延伸; ISUP = 国际泌尿外科病理学会;磁共振成像;PSA =前列腺特异性抗原;SVI =精囊侵犯。
基于外部验证的预测模型中预测因子的系数,研究者们确定了四个新的风险类别。
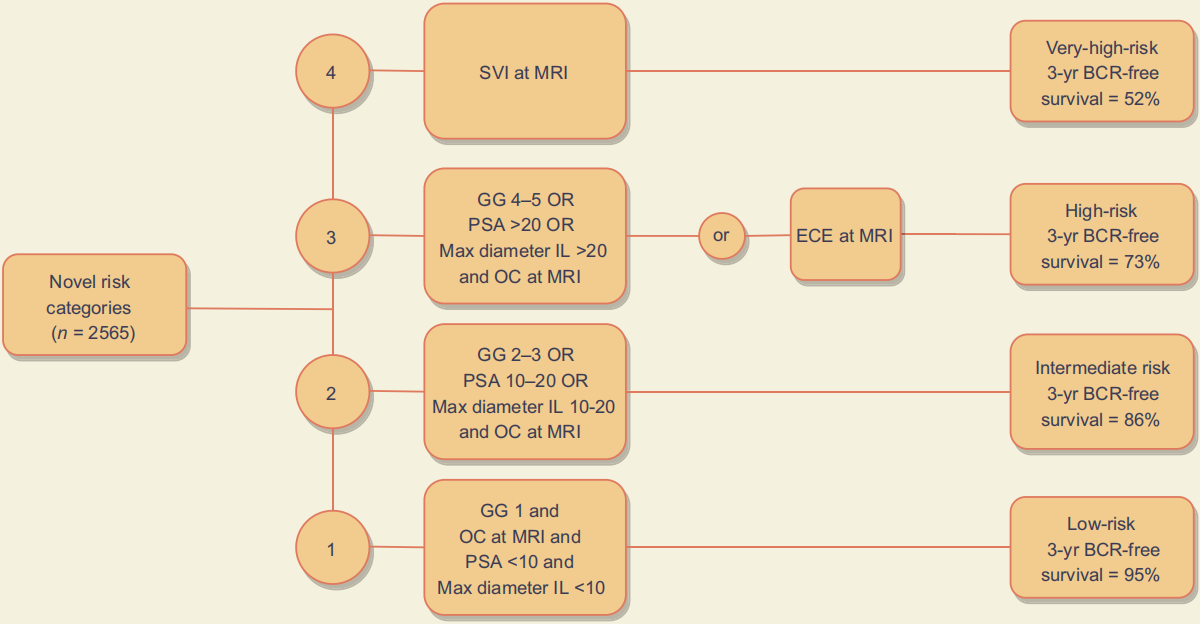
图2 新的风险分类根据分级组、MRI分期、MRI指标病灶最大直径和术前PSA将患者分为四类。
BCR =生化复发;ECE =囊外延伸;GG =病理等级分组;IL =指标病变(index lesion);磁共振成像;OC =器官受限;PSA =前列腺特异性抗原;SVI =精囊侵犯
前列腺癌患者按照新危险分类进行分层后bcr情况(图3)
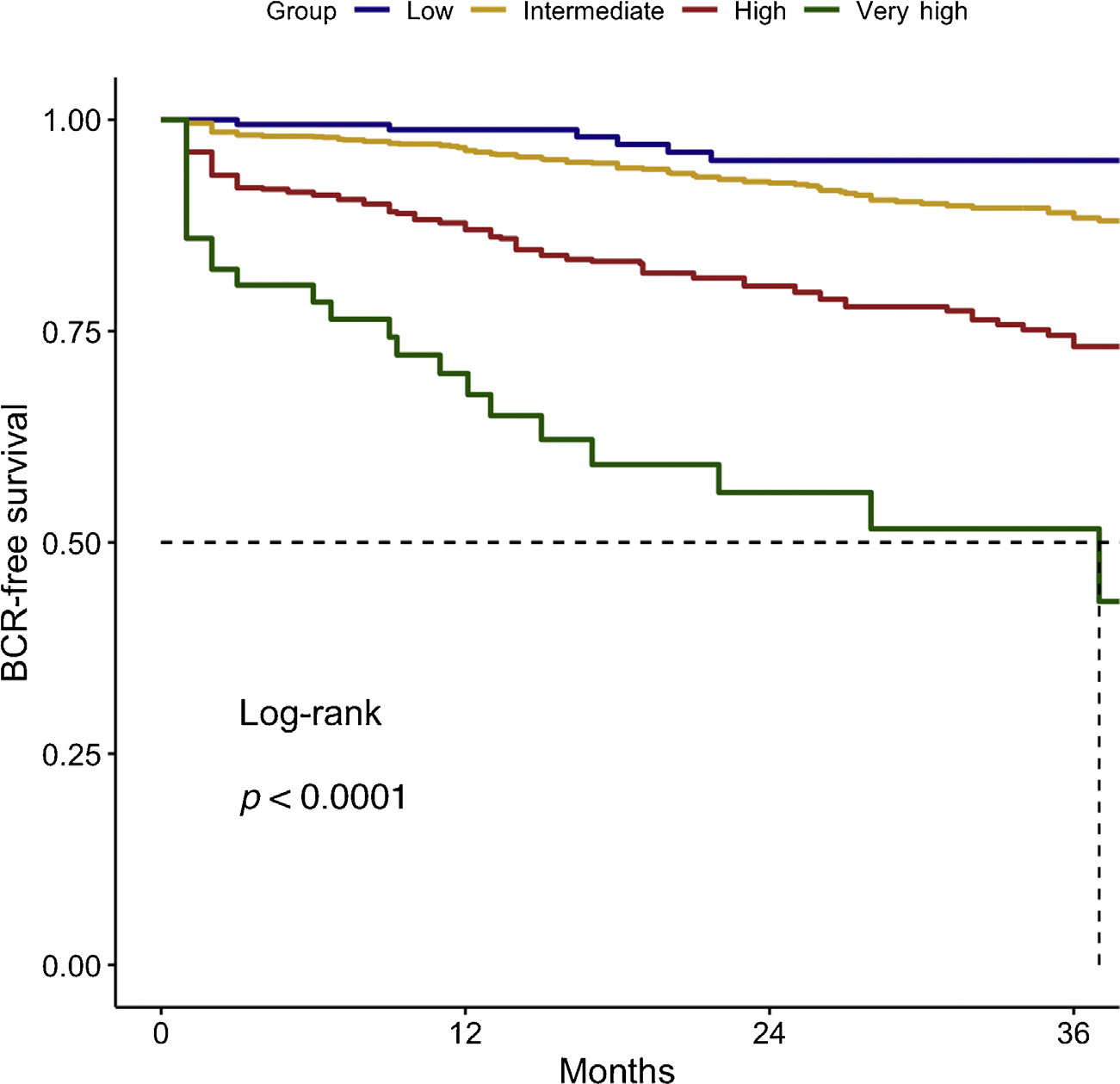
图3 Kaplan-Meier分析报告了前列腺切除术后前列腺癌患者按照新危险分类进行分层后bcr生存。BCR =生化复发。
结论
该研究开发并外部验证了新的风险类别,整合了临床和放射学参数来预测早期BCR。在预测早期BCR方面,分层工具显示出比现有工具更高的准确性,应该用于协助医生进行术前咨询和治疗选择。
文献来源:Mazzone E, Gandaglia G, Ploussard G, et al. Risk Stratification of Patients Candidate to Radical Prostatectomy Based on Clinical and Multiparametric Magnetic Resonance Imaging Parameters: Development and External Validation of Novel Risk Groups. Eur Urol. 2021 Aug 13:S0302-2838(21)01930-8. doi: 10.1016/j.eururo.2021.07.027. Epub ahead of print. PMID: 34399996.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#切除术#
44
#根治性切除术#
33
#筛选#
45
#根治#
27
学习
58
大楼咯我了
48
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
50
不错学习了
66
学习学习
43
好。学习
29