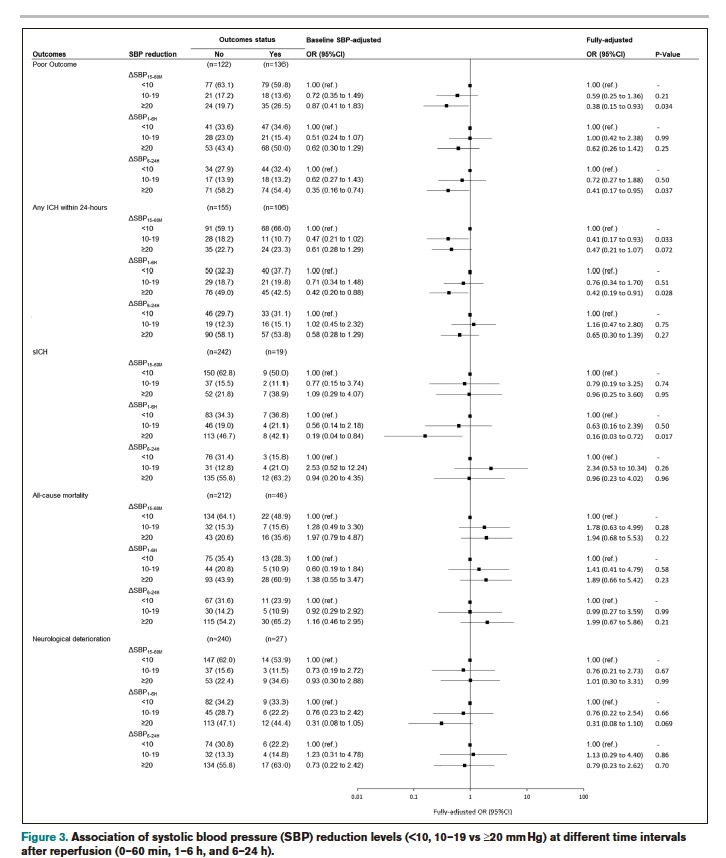
血管内治疗(EVT)彻底改变了大血管闭塞导致的急性缺血性中风的治疗方法。尽管再通率很高,但大约一半的治疗患者在EVT后没有实现功能独立。高血压(BP)在EVT后很常见,并被认为在再灌注损伤中发挥作用,这使其成为潜在的治疗目标。观察性研究一再表明,高血压和成功再灌注后的不良结果之间存在关联,这一发现也得到了临床前研究的支持。
 然而,高血压与卒中后不良预后之间的因果关系尚未得到证实,而且缺乏支持EVT后降压获益的证据。虽然,降压治疗可以减轻成功再灌注后的再灌注损伤,但它有可能加重半脑组织的低灌注,尤其是在不完全再灌注的情况下。
然而,高血压与卒中后不良预后之间的因果关系尚未得到证实,而且缺乏支持EVT后降压获益的证据。虽然,降压治疗可以减轻成功再灌注后的再灌注损伤,但它有可能加重半脑组织的低灌注,尤其是在不完全再灌注的情况下。
因此,在成功再灌注后降低血压的安全性和有效性的平衡上仍存在不确定性。先前的观察性研究也暗示了在EVT后降低收缩压(SBP)的潜在益处,并且没有安全问题。然而,最近发表的BPTARGET试验(Blood Pressure Target in Acute Stroke to Reduce Hemorrhage After Endovascular Therapy)表明,与指南推荐的血压控制(SBP,<185 mm Hg)相比,在接受EVT治疗的患者中,强化降压策略(SBP目标100-129 mm Hg)的结果是中性的,这些患者在手术结束时已经成功实现了再灌注。
藉此,法国Hôpital Fondation Ophtalmologique Adolphe de Rothschild 的Mohammad Anadani等人,对BP-TARGET试验数据进行了事后分析,以评估不同时间间隔的ΔSBP与临床和影像学结果之间的关联,并评估成功再灌注后的头24小时内,不同程度的SBP降低对出血性并发症和不良结局风险的治疗效果变化。
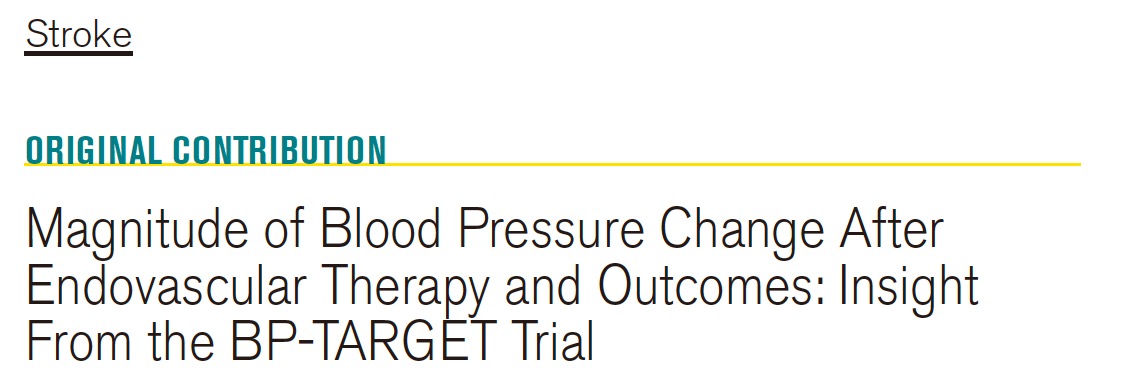
该研究是BP-TARGET多中心试验(Blood Pressure Target in Acute Stroke to Reduce Hemorrhage After Endovascular Therapy)的一项事后分析。ΔSBP被定义为手术结束时的SBP减去不同时间间隔(手术后15-60分钟、1-6小时和6-24小时)的平均SBP。主要结果是功能不良的结果(90天修正的Rankin量表评分3-6)。
他们共纳入了267名患者(130名在强化治疗组)。与结果良好的患者相比,结果不佳的患者在所有时间间隔内都有较低的ΔSBP(SBP降低较少)。
在调整了包括基线SBP在内的潜在混杂因素后,ΔSBP_15-60M和ΔSBP_6-24H都与较低的不良结局几率有关(调整后的几率比每减少5mmHg SBP,分别为0.89[95%CI,0.81-0.99],以及调整后的几率比0.82[95%CI,0.73-0.92])。
 关于安全结果,脑实质出血的患者在所有时间间隔内的ΔSBP都较低。ΔSBP_15-60M与任何脑实质内出血的几率较低有关(调整后的几率比每降低5mmHg SBP为0.91[95% CI, 0.83-0.99])。
关于安全结果,脑实质出血的患者在所有时间间隔内的ΔSBP都较低。ΔSBP_15-60M与任何脑实质内出血的几率较低有关(调整后的几率比每降低5mmHg SBP为0.91[95% CI, 0.83-0.99])。
相反,在任何时间间隔内,ΔSBP与死亡率或神经系统恶化无关。
该研究的重要意义在于发现了: 在成功的再灌注后,ΔSBP与不良结局呈线性关系,从基线SBP下降越少,不良结局的风险就越高。
原文出处:
Anadani M, Maïer B, Escalard S, et al. Magnitude of Blood Pressure Change After Endovascular Therapy and Outcomes: Insight From the BP-TARGET Trial. Stroke. Published online February 3, 2022:STROKEAHA.121.036701. doi:10.1161/STROKEAHA.121.036701
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#收缩压#
53
受益匪浅
48
学习了!
55
学习了
52
#取栓#
57