【一般资料】
患者男,61岁
【主诉】
因“右侧腰腿痛4个月,加重1个月”于2016年11月29日入院
【现病史】
患者入院前4个月无明显诱因出现右侧腰背痛,向右下肢放射,休息后能缓解。1个月前开始右下肢疼痛明显加重,伴麻木感,不能久站,平卧不能缓解,予对症治疗效果不佳。患者于2015年4月13日因“左上肺占位”行“左上肺切除+淋巴结清扫”手术治疗,术后病理检查示“肺腺癌Ⅱ级”,术后患者恢复良好,接受4个疗程“培美曲塞+顺铂”的化疗,并于术后3个月接受术后瘤床及淋巴引流区姑息性放疗,共完成PTV50GF/2Gy/25F,之后于胸外科定期复查胸部CT,未见肿瘤复发征象。
【体格检查】
下腰椎棘突叩痛(+),右小腿内侧浅感觉减退,右下肢股四头肌和胫前肌肌力均为4级,左下肢肌力、感觉正常,双下肢生理反射存在,病理反射未引出,鞍区感觉存在。
【辅助检查】
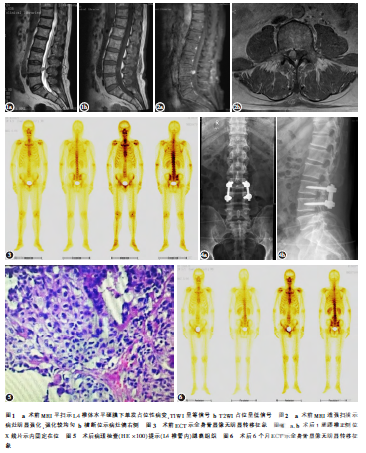
影像学检查:腰椎MRI平扫提示L4节段椎管内类圆形结节影,大小约1.0×0.8CM,T1WI呈等信号,T2WI呈低信号,增强MRI显示病灶明显强化且强化较均匀(图1、2),考虑神经源性肿瘤可能性大。头颅及颈胸椎MRI未见其他转移性病灶;肺部CT示左肺上叶切除术后改变,两肺纤维化病灶、胸膜肥厚;ECT示全身骨显像未见明显骨转移征象(图3)。
【初步诊断】
诊断为“L4椎管内硬膜下占位,左肺腺癌术后”,占位性质考虑神经源性肿瘤可能,转移性肿瘤不除外。
【治疗】
因患者肺癌术后一般情况良好,随访无复发和全身转移征象,腰腿痛症状考虑为腰椎管内占位引起,保守治疗无效,遂考虑行手术治疗。进一步排除手术禁忌后于2016年12月2日在全身麻醉下行腰后路椎管内肿瘤切除内固定术。术中见肿瘤位于L4椎体水平,硬膜下右侧,约1.0×1.0×0.8CM大小,形状不规则,质软,有包膜,黄白色,与脊膜无粘连,与马尾神经粘连明显,仔细分离后切断小部分粘连神经纤维,完整将肿瘤组织取出后送病理检查,肿瘤切面为鱼肉样。术后常规预防感染、营养神经等治疗,患者术后右侧腰腿痛明显缓解,下肢肌力、感觉较术前无明显变化,术后1周复查腰椎X线片显示内固定在位(图4)。术后病理检查:角蛋白(Cytokeratin,CK)(+)、CK(AE1/AE3)(+)、CK20(-)、甲状腺转录因子1(TTF-1)(+)、新型天门冬氨酸蛋白酶A(Napsin-A)(+)、尾型同源框基因转录因子2(CDX2)(-)、绒毛蛋白(Villin)(-)、精氨酸酶1(Arginase1,Arg-1)(-)、CK5/6(-)、P63(-),提示(L4椎管内)腺癌组织(图5),结合免疫组化和病史符合肺癌转移。诊断为L4椎管内硬膜下肺癌转移瘤,患者出院后未再接受放化疗,术后半年随访无明显腰腿痛症状,复查胸部CT未见肿瘤复发征象,复查ECT全身骨显像未见明显骨转移征象(图6),嘱患者术后1年再次复查。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#硬膜下#
35
#腰椎管内#
34
#椎管内#
27
#椎管#
23
#转移瘤#
25
比较少见的转移.对于规则治疗后的转移.要从传统转移中分出来
36
#腰椎#
28
#腰椎管#
27
#癌转移#
30
学习一下
51