Cell Rep:移除“书签”为获得诱导多能干细胞铺平道路
2016-09-22 佚名 生物谷
近日,来自美国阿拉巴马大学的研究人员在国际学术期刊Cell Reports上发表了一项最新研究进展,他们找到利用化合物促进体细胞重编程获得诱导多能干细胞的新方法。虽然人体内200多种不同的细胞类型具有相同的基因组,但是每种细胞类型都存在独特的基因表达程序。在体细胞重编程获得诱导多能干细胞的过程中,清除原始细胞的体细胞转录程序是一个关键事件。在这项研究中,研究人员找到了一种新策略,他们利用小分子化合

近日,来自美国阿拉巴马大学的研究人员在国际学术期刊Cell Reports上发表了一项最新研究进展,他们找到利用化合物促进体细胞重编程获得诱导多能干细胞的新方法。
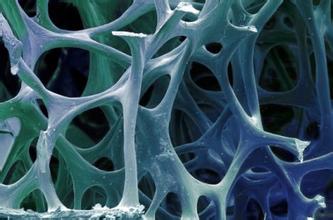
虽然人体内200多种不同的细胞类型具有相同的基因组,但是每种细胞类型都存在独特的基因表达程序。在体细胞重编程获得诱导多能干细胞的过程中,清除原始细胞的体细胞转录程序是一个关键事件。
在这项研究中,研究人员找到了一种新策略,他们利用小分子化合物干扰体细胞的转录记忆帮助体细胞重编程获得多能干性。研究人员发现靶向BET家族蛋白乙酰赖氨酸结合口袋的小分子化合物能够大大增强重编程过程。更进一步研究表明小分子化合物靶向BET的bromodomains能够下调或关闭成纤维细胞的体细胞基因表达,还会在重编程早期阶段导致成纤维细胞形态丧失。
研究人员提出了一个用于解释实验结果的模型:在正常的细胞分裂过程中,活跃的成纤维细胞基因在有丝分裂时期因为BET蛋白与乙酰化的染色质结合被打上标签,而RNA 聚合酶II则从染色质上脱落。在细胞分裂间期开始的时候,这些标签会指导聚合酶回到需要转录的基因上,随后开始基因的转录。而加入化合物抑制剂之后,因小分子化合物与BET蛋白的结合,在有丝分裂阶段活跃的成纤维细胞基因被去掉标签,这会导致成纤维细胞相关基因的表观遗传记忆被清除,当重新进入细胞分裂间期,与成纤维细胞有关的基因转录无法启动,增强了体细胞重编程变为诱导多能干细胞的能力。
综上所述,研究人员通过实验证明借助靶向BET bromodomains的化合物清除体细胞的转录记忆可以促进细胞发生命运转变。该研究为提高诱导多能干细胞的得率提供了一个新策略。
原始出处
Zhicheng Shao1, 5, Chunping Yao1, 3, 5, Alireza Khodadadi-Jamayran1, 5, Weihua Xu4, Tim M. Townes1, Michael R. Crowley2, Kejin Hu.Reprogramming by De-bookmarking the Somatic Transcriptional Program through Targeting of BET Bromodomains.Cell Rep.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
35
#Cell#
26
#诱导多能干细胞#
30
cell牛逼。。
35
谢谢分享!
46
继续关注!
47
学习了谢谢。
32
了解一下!
43