AP&T: 溃疡性结肠炎的内镜愈合对组织学缓解的预测作用
2020-08-31 MedSci原创 MedSci原创
根据最近的临床研究,UC患者的推荐治疗目标是达到是直肠无出血,大便次数正常,内镜下粘膜愈合的多项指标。
根据最近的临床研究,UC患者的推荐治疗目标是达到是直肠无出血,大便次数正常,内镜下粘膜愈合的多项指标。大约50%-60%的UC患者达到内镜缓解后也可以达到组织学缓解。那么具体有多少患者可以获得组织学缓解目前还没有明确的研究证实,本项研究旨在评估以内镜治疗为目标的溃疡性结肠炎患者的预测指标和实现组织学缓解的结果。

研究人员对患有活动性溃疡性结肠炎(改良的梅奥内窥镜评分2或3)的成人进行了一项回顾性队列研究,这些患者治疗经过反复优化以实现内窥镜愈合。我们使用Cox比例风险分析确定了实现组织学缓解的预测因素。

在411例临床活动性溃疡性结肠炎患者中,有270例获得了内镜治愈。在270名患者中,有55%同时达到了组织学缓解。最终内镜评估时内镜愈合的深度是组织学缓解的唯一独立决定因素。在28个月内,达到组织学缓解的临床复发风险较低(1年累积风险:18.7%vs 29.5%;OR:0.56 [0.37-0.85]),住院风险也较低(OR:0.44 [0.20-0.94])。
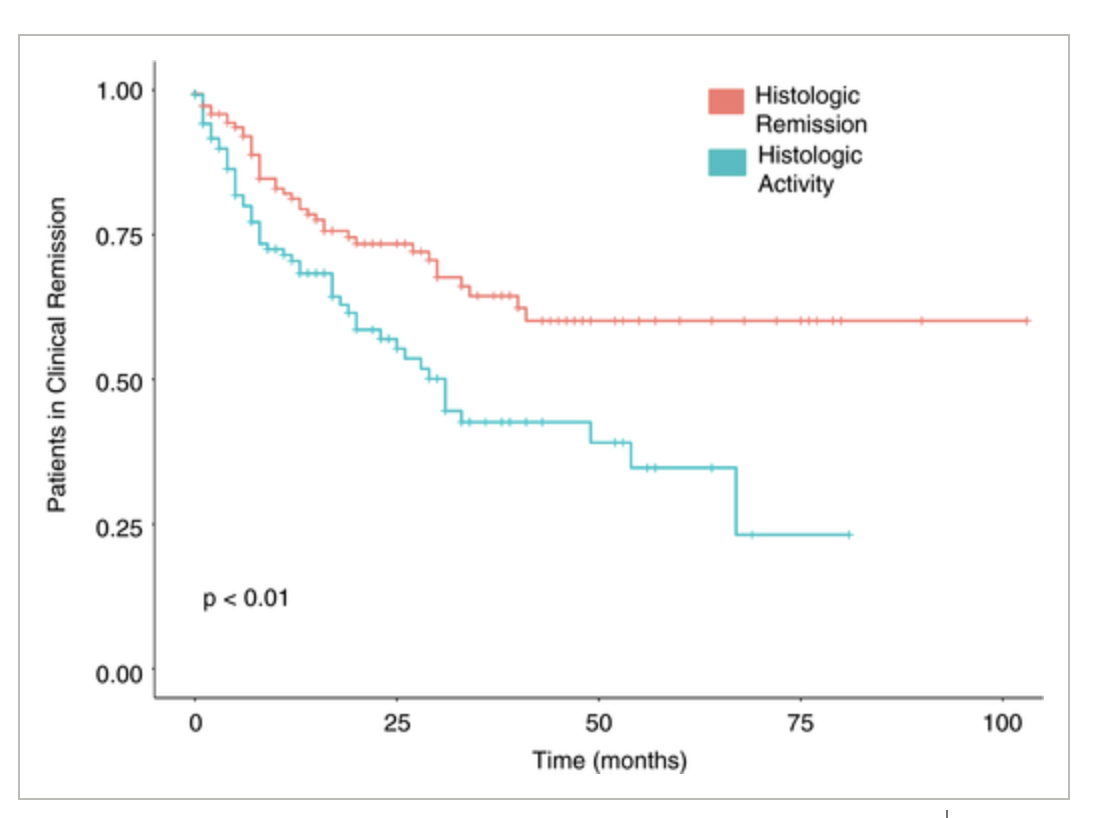
本项研究结果证实在以内镜治愈为目标的活动性溃疡性结肠炎患者中,有55%的患者可以同时达到组织学缓解。组织学缓解,特别是在改良Mayo内窥镜评分达到1的患者中与良好的预后相关。
原始出处:
Sushrut Jangi. Et al. Predictors and outcomes of histological remission in ulcerative colitis treated to endoscopic healing. Alimentary Pharmacology and Therapeutics.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#溃疡性#
23
#组织学#
36
#内镜#
36
学习
79
了解
90