Blood:转录因子ATF4激活BCL11A转录以沉默胎儿血红蛋白表达
2020-05-01 QQY MedSci原创
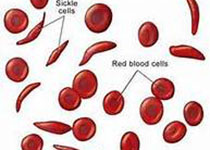
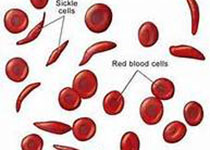
HRI激活ATF4,促进BCL11A转录和胎儿血红蛋白沉默。 ATF4以物种选择性方式调控BCL11A。
本研究通过CRISPR-CAS9导向的人红细胞功能丧失性筛查,确定了转录因子ATF4,一个已知的受HRI调节的蛋白,是一种新的γ-珠蛋白调节因子。
ATF4通过与γ-珠蛋白转录抑制因子BCL11A的增强子结合并促进BCL11A的增强子-启动子接触,直接刺激BCL11A的转录。值得注意的是,HRI缺陷小鼠表现出正常的Bcl11a水平,这表明了物种选择性调节,研究人员通过证明小鼠Bcl11a增强子上存在一个在很大程度上都是可有可无的类似的ATF4基序来解释了这一点。
综上所述,本研究揭示了从HRI到ATF4再到BCL11A到γ-珠蛋白的线性信号通路,并阐明了小鼠珠蛋白基因调控模型的潜在局限性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#转录#
31
#胎儿血红蛋白#
48
#蛋白表达#
37
#转录因子#
47
#ATF4#
44