Eur J Cancer:奥沙利铂/卡培他滨联合放疗(OxCapRT)对比紫杉醇/卡铂联合放疗(CarPacRT)新辅助治疗对可切除食管腺癌的疗效和安全性:NeoSCOPE长期随访结果
2021-06-25 yd2015 MedSci原创
对于可手术切除的食管腺癌患者,紫杉醇/卡铂联合放疗对比奥沙利铂/卡培他滨联合放疗作为新辅助治疗有OS和PFS获益。同时,远处转移较局部复发更常见。
NeoSCOPE是英国开展的一项开放标签、多中心、随机、II期试验。纳入2013年10月至2015年2月 cT3 and/or cN1 (TNM v7)可手术切除的食管腺癌(OAC)或胃食管连接处(GOJ)腺癌患者。评估奥沙利铂/卡培他滨联合放疗(OxCapRT)对比紫杉醇/卡铂联合放疗(CarPacRT)用于此类患者术前新辅助治疗的疗效和安全性。主要研究终点为病理完全缓解率(pCR),次要研究终点为毒性,PFS、OS和进展模式。2017年已经报道,CarPacRT组和OxCapRT组的pCR率分别为29.3%和11.1%。近期,European Journal of Cancer杂志发表了长期随访的结果。

研究纳入85例患者,两组中位随访时间分别为43.4个月 (95% CI: 37.7-53.6) 和51.0个月 (95% CI: 45.5-54.3)。 OxCapRT组中位OS为41.7个月(95%可信区间[CI] 19.6至未达),而CarPacRT组中位OS未达到(HR = 0.48, 95% CI: 0.24 -0.95, P= 0.035)。OxCapRT组的3年和5年的OS率分别为52% (95% CI: 35%-67%)和 39% (95% CI: 21%-56%); CarPacRT组的3年和5年的OS率分别为 74% (95% CI: 58%-85%) 和54% (95% CI: 33%-70%)。按肿瘤退缩级别(TRG)分为TRG3/4和TRG1/2两组,TRG3/4组患者中位OS为49.6个月 (95% CIs: 30.1 to not reached) ,而TRG 1/2组患者中位OS未达到,两组没有统计学差异 (HR=1.49, 95% CI: 0.70-3.17, P =0.301)。

os
OxCapRT组中位无进展生存期(PFS)为32.6个月(95% CI: 17.1-未达到), 而CarPacRT组中位无进展生存期(PFS)未达到(HR= 0.54, 95%CI: 0.29-1.01, P= 0.053)。两组的1年PFS率为68% [95% CI: 52-80] vs 81% [95% CI: 66-90]), 3年PFS率为47% [95% CI: 30-61] vs 63% [95% CI: 47e75]) 以及 5 年PFS率为19%[95% CI: 2e51]) vs 51% [95% CI: 32e67])。在两组中,出现远处转移进展是局部进展的两倍。
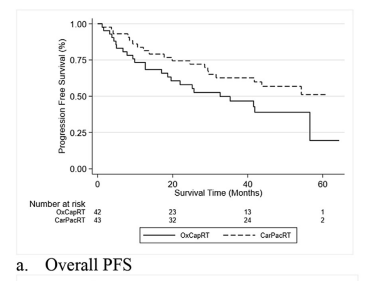
PFS
在6个月时,OxCapRT组观察到更多的3/4级毒性反应,为15% 对比3%,但是没有统计学差异(p=0.069)。
综上,对于可手术切除的食管腺癌患者,紫杉醇/卡铂联合放疗对比奥沙利铂/卡培他滨联合放疗作为新辅助治疗有OS和PFS获益。同时,远处转移较局部复发更常见。
原始出处:
Somnath Mukherjee , Christopher Hurt , Ganesh Radhakrishna,et al. Oxaliplatin/capecitabine or carboplatin/paclitaxel-based preoperative chemoradiation for resectable oesophageal adenocarcinoma (NeoSCOPE): Long-term results of a randomised controlled trial. Eur J Cancer. 2021 Jun 19;153:153-161. doi: 10.1016/j.ejca.2021.05.020. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
27
#随访结果#
39
#CARP#
30
#疗效和安全性#
26
#新辅助#
26
#CAP#
50
#联合放疗#
37
#铂#
31
#食管腺#
45
#长期随访#
44